Alavert
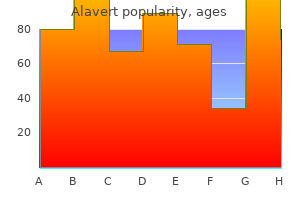
Alavert dosages: 10 mg
Alavert packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills
Alavert 10 mg buy low cost
The surgeon may elect to use a free-hand approach or one of several technical adjuncts to assist in optimal catheter placement (ultrasound allergy treatment non drowsy discount 10 mg alavert otc, endoscope allergy forecast nc cheap alavert 10 mg on-line, image-guidance, and so on. The distal catheter is handed from the cranial incision to a ~1 cm incision made in the abdomen at a website chosen by the surgeon, primarily based on affected person anatomy or different elements (presence of gastrostomy tube or surgical scars). A parietal passing incision may be required to deliver the distal catheter from an anterior entry level to the abdominal incision. Peritoneal entry could also be achieved via mini-laparotomy, laparoscopy, minimally invasive port or trocar, or different technique. After peritoneal access is established, the shunt is totally assembled, securing both the ventricular and distal catheters to the valve. The valve itself fits within a subgaleal pocket common for this purpose, and after verification of shunt patency and function the distal catheter is fed into the peritoneum. In common, ~30 cm of intraperitoneal tubing is implanted in babies to allow for continued development. Use of an anterior versus posterior entry website for the ventricular catheter remains a subject of investigation. Propensity for under- or over-drainage, surgeon preference/experience, and the perceived want for valve setting adjustments usually inform valve choice. Aftercare Sterile dressings may be placed after shunt insertion, which may be eliminated 24 to 48 hours post-operatively. Sagittal T1 (A), axial T1 through the lateral ventricles (B), and axial T1 by way of the fourth ventricle (C) images show a dramatic discount and near-normalization in ventricular measurement. Additional common appointments are sometimes scheduled on a a number of month-to-month or annual foundation. The most typical cause of shunt malfunction is proximal obstruction of the ventricular catheter, likely from reduced ventricular dimension and/or ingrowth of the choroid plexus. Exceptinrare instances, shunt malfunction requires urgent surgical revision of the shunt. Shunt infection could also be associated with ventriculitis, scarring and loculation of the ventricles, neurological morbidity, and, not often, death. Risk elements for shunt infection embrace younger age (<6 months), presence of gastrostomy tube, and prior neurosurgery. Clinically, sufferers could complain of headaches, typically postural, nausea, and vomiting. Neuro-imaging usually demonstrates small ventricles and, if distinction is run, potentially meningeal enhancement. Chronic over-drainage is associated with slit-ventricle syndrome, a condition that causes disabling and often difficult-to-treat complications. Overdrainage is usually treated by revising the shunt to a higher stress or flow-control system with an anti-siphon gadget. Many modern shunts have been designed with onboard programmable differential pressure valves, anti-siphon gadgets, or flowregulated valves to help address this drawback. Although rare, intracranial hemorrhage (epidural, subdural, intra-parenchymal, or intraventricular) may occur as a complication of shunt placement. While such hemorrhages usually resolve spontaneously without any further intervention, they might be related to a higher price of subsequent shunt obstruction and malfunction, especially in cases of intraventricular hemorrhage. Mechanical shunt failure requires surgical revision and is most commonly attributable to proximal obstruction. Problems with over-drainage could be managed with higher-pressure or programmable valves, anti-siphon units, or flow-regulated valves. Evidence and Outcomes Hydrocephalus is the most typical surgically treatable neurological problem within the pediatric population. There stays little info on long-term outcomes, and specifically high quality of life or practical outcomes, in handled kids. A current quantity of Journal of Neurosurgery: Pediatrics was dedicated to establishing pediatric hydrocephalus remedy pointers through systematic reviews of available evidence. There is an urgent want for standardized devices and care pathways, similar to 8 Communicating Hydrocephalus those created through the Hydrocephalus Clinical Research Network, to inform each medical therapy and analysis for this condition. Ventricular catheter entry site and never catheter tip location predicts shunt survival: a secondary evaluation of three large pediatric hydrocephalus research. Effect of electromagnetic-navigated shunt placement on failure rates: a prospective multicenter examine. Risk components for first cerebrospinal fluid shunt infection: findings from a multi-center potential cohort examine. Lack of advantage of endoscopic ventriculoperitoneal shuntinsertion: amulticenterrandomizedtrial. Baird Case Presentation 2 A 12-year-old boy presents to his pediatrician with a 2 month historical past of fatigue, blurry imaginative and prescient, and steadiness difficulties while walking. He endorses intermittent mild complications, and his dad and mom notice issue with short-term memory and worsening college efficiency over the earlier 6 months. The historical past of neurocognitive decline, imaginative and prescient change, and gait dysfunction support this prognosis. It is essential to establish the etiology of the hydrocephalus each time potential, because the underlying diagnosis will influence the remedy plan, prognosis, and household counseling. Communicating hydrocephalus, ventriculomegaly ex vacuo, and benign familial macrocrania should also be considered, although these are much less probably within the absence of a dilated fourth ventricle. In addition, the affected person ought to undergo a full ophthalmological evaluation to assess for any visible compromise current pre- operatively and for post-treatment follow-up to ensure full resolution of the papilledema. These findings are according to a analysis of obstructive hydrocephalus secondary to aqueductal stenosis. The underlying etiology of newly diagnosed hydrocephalus ought to be established to determine the suitable intervention and to accurately counsel the household relating to prognosis. Preoperative funduscopic analysis ought to be carried out with any new analysis of hydrocephalus, and if papilledema or visible impairment is suspected, an pressing referral to ophthalmology should be placed. Which surgical treatment choices are available for the management of obstructive hydrocephalus Which anatomic structures have to be fastidiously assessed to have the ability to decide candidacy for endoscopic therapy Decision Making the presence of papilledema secondary to elevated intracranial strain can outcome in additional visual decline, which might end in permanent deficit. While shunt placement is an effective choice, it carries higher lifetime danger of morbidity, including post-operative shunt an infection, need for additional surgery in the setting of a shunt malfunction, and overdrainage problems. Endoscopic choices for the therapy of obstructive hydrocephalus ought to be thought-about each time the anatomy is amenable. How would the efficacy of an endoscopic third ventriculostomy be affected by the invention of occlusive cisternal membranes
Alavert 10 mg order with mastercard
A double-J stent is then placed according to allergy and treats cheap alavert 10 mg visa ureteral size along the anastomosis just earlier than closure and left in place for four to 6 weeks to keep away from obstruction and extravasation allergy treatment for pollen cheap alavert 10 mg fast delivery. All anastomoses must be covered with peritoneum or omentum if potential to enhance therapeutic. The surgeon should resolve on the method (intravesical and extravesical) and the necessity for additional procedures to complement a shortened ureter. A useful gizmo to examine ureteral length, and due to this fact to create a tension-free anastomosis, is bladder distention with saline by way of the catheter if no cystotomy is present. If a cystotomy has been made, then an intravesical or transvesical approach can simply be carried out by way of this opening, unless in an ectopic space, or a brand new cystotomy may be made along the dome for adequate visualization of the trigone. We suggest filling of the bladder first to capability, then inserting a 2-0 Vicryl stay suture (full thickness if possible) on either facet of the future cystotomy. This permits for elevation of the surrounding bladder wall and appropriate visualization of the bladder mucosa as the bladder deflates. A stent of appropriate length is placed earlier than closure of the anastomosis, and a catheter is left throughout the bladder for 10 to 14 days, depending on surgeon desire, to permit for full therapeutic of the anastomosis and cystotomy. If potential, fine Sarot or Metzenbaum scissors can be used to bluntly make the tunnel by way of the bladder wall by coming into the adventitia and then moving inferiorly alongside the detrusor muscle and exiting intravesically at a determined length. An Overholt clamp is then used to grasp the stay suture at the end of the ureter and pull it through the defect; then the anastomosis can be carried out intravesically. The serosal layer is then mounted to the ureteral wall with two or three delayed absorbable sutures to decrease pressure. Another choice is to make the cystotomy directly via the bladder wall after which place imbricated stitches utilizing the bladder detrusor and serosal layers to create resistance to reflux. Again, tension-free anastomoses are key, and a ureteral stent is positioned throughout the new anastomosis. For inadequate ureteral size, the surgeon may have to mobilize the bladder on the contralateral side, possibly by controlling some or all of the bladder pedicle on that contralateral facet, because the bladder will still retain significant collateral blood provide. This can be carried out with a vesselsealing instrument or 0 or 2-0 silk suture ties, with care taken to not injure the contralateral ureter. In this case, it is important to maximally mobilize the bladder contralaterally and take a look at bladder capability earlier than forming the tubularized section of the dome that will be swung cephalad to meet the distal ureter for anastomosis. The length between the bladder wall and the distal ureter is measured to find a way to make a tension-free anastomosis. The base of the Boari flap is positioned alongside the posterior wall, just inferior to where a direct line could be drawn from the bladder to the ureteral finish. The flap is then marked out with either stay sutures or a Bovie cautery device, leaving 3 to 4 cm width for the bottom. Many surgeons create a rhomboid form with a wider base and narrower tip to accommodate for ureteral circumference. The flap is then released from the bladder on all sides except the bottom and tubularized and swung as much as meet the ureter. For the ureteral anastomosis and tubularization, 4-0 Vicryl or delayed absorbable suture is used. The ureteral stent is left in situ for 4 to 6 weeks and a Foley catheter for 10 to 14 days to permit for maximal drainage and therapeutic. A postoperative cystogram can be obtained in accordance with surgeon desire before removal of any catheters. Advanced Reconstructive Procedures More advanced reconstructive procedures for giant ureteral defects or complete ureteral loss embody procedures such as transureteroureterostomy, renal autotransplantation, and ileal substitution. Contraindications to transureteroureterostomy embrace insufficient donor ureter size, and illness of the recipient or donor ureter similar to urothelial carcinoma, metastasis involving the ureter or ureteral fibrosis, history or presence of renal stones, and lack of ability to obtain a tension-free anastomosis. This must be carried out solely sparingly because of the potential for issues, quoted by the authors of one study of sixty three sufferers to have occurred in up to 24%. Renal autotransplantation can additionally be very rarely indicated and requires experienced transplant surgeons for harvesting and timely anastomosis of the renal unit. Other uses of ileum embody bladder augmentation or ileal conduit formation or continent urinary diversion (see Chapter 21). One small retrospective research by Wilkin and colleagues at the University of Wisconsin assessed the effect of pelvic radiation on continent cutaneous urinary diversions. Significantly more complications have been seen in the irradiated group than in the nonirradiated group (83% vs. In well-selected circumstances, endoscopic and other minimally invasive procedures have shown success. Liatsikos and colleagues described a examine of 10 sufferers with 12 obstructed renal units as a result of ureteral stenosis after a gynecologic surgical procedure. Balloon dilation should be managed as a result of it could appropriately enlarge the lumen; nevertheless, ureteral rupture also can take place, and distinction material can act as an irritant to the retroperitoneum and instigate future fibrosis and stricture formation. Another possible therapy is the endoscopic "ureteral rendezvous," which typically requires a radiologist and a urologist. The second layer consists of the serosal layer, once more closed in a working trend. We choose to use 3-0 Vicryl for the first layer and 2-0 Vicryl suture for the second. Once the bladder has been repaired, the catheter should remain for 1 to 2 weeks relying on surgeon preference and ease of restore however could be left for longer durations, particularly in patients with giant and complex bladder defects and in sufferers with a historical past of pelvic irradiation. Ideally, a cystogram must be obtained to confirm complete bladder therapeutic earlier than Foley removal. Fistula Complications Formal analysis of fistulas could be performed in a medical setting or in an operative setting. Certainly, a high degree of suspicion is important when a patient has constant vaginal leakage or constant urinary incontinence after a historical past of pelvic surgery or irradiation. In the scientific setting, a pelvic examination can typically permit identification of enormous fistulas with simple palpation and appropriate lighting. For smaller fistulas, or those not purely from the bladder, further research such because the "tampon test" or "three-sponge take a look at" could be carried out. During these tests methylene blue or indigo carmine is placed throughout the bladder by utilizing a Foley catheter, with (tampon test) or with out (three-sponge test) using oral Pyridium (phenazopyridine) to stain the ureteral urine earlier than it enters the bladder. Simple wetting (no dye coloration) of the top swab raises concern for a ureterovaginal fistula. Discoloration of the bottom swab signifies either introital backflow or a urethral fistula. Instead, most surgeons merely carry out thorough examinations with the patient underneath anesthesia, when cystoscopy, vaginoscopy, and retrograde pyelograms may be performed with out patient discomfort or time constraints. This would also allow for biopsy of the fistulous tract if malignant involvement is suspected. Surgically induced fistulas seem to have a unique time course and pure history than radiation-induced fistulas. Surgically induced fistulas tend to manifest earlier and have less tissue change over time. Commonly, conservative management is attempted first, similar to catheter drainage for several weeks for small fistulas.
Generic 10 mg alavert otc
The contribution to the corticospinal tracts are less well visualized with our methods allergy testing list alavert 10 mg generic with amex. Finally food allergy symptoms 3 year old alavert 10 mg generic free shipping, the decrease motor cortex principally communicates with the center motor cortex, as properly as premotor, and sensory cortices. Its lengthy range fibers mostly run within the coronal aircraft, and it has only smaller U-fiber connections with adjoining cortices anterior and posterior to it. With these exceptions in mind, the cingulum in any other case is a protracted connection interconnecting the basal forebrain and septal constructions with the cingulate gyrus cortex, finally terminating within the parahippocampal gyrus. Connections to the Deep Structures Caudate Nucleus the vast majority of the majority of the caudate nucleus is situated within the head. The anterior peduncle passes through the anterior limb of the interior capsule and heads to the anterior frontal lobe. The posterior peduncle begins simply anterior to the atrium and hooks round it on its approach to the occipital lobe. It is carrying the optic radiations, as well as bidirectional communications between the visible system and the thalamus. The inferior peduncle is considerably shorter, and is headedto the orbitofrontal cortices, the amygdala and insula. Crossing Points Moving back to the macro scale, it is necessary to make a couple of general observations about world tract patterns that are critical to understanding cerebral anatomy and tips on how to plan safe surgeries. Another crossing point occurs deep to the posterior components of inferior and center frontal gyrus, particularly close to the airplane of the anterior insula. This for my part is among the nice cofounding issues with using lesion information to ascribe operate to particular cortical areas, as lesions at crossing points have the power to cause widespread community injury with small lesions. Final Points that is essentially the most detailed evaluation of specific white matter anatomy that I am aware of to date. This is just a detailed set of images not out there wherever else at present, which begin the discussions which observe. Functional Networks of the Human Cerebrum Playlist Quick entry IntroductionMethods and AssumptionsSpeech NetworkThe Anatomy of the NetworkPraxis SystemThe Neglect NetworkVisual SystemRamifications of the Visual Network Anatomy for SurgeryAttention NetworksThe Large-scale Executive NetworksFinal ObservationsReferences Introduction In this article, I take the bold step of attempting to cobble connectomic data into a coherent mannequin of human brain networks. It ought to be acknowledged that by doing so, I am placing out some information which can have to be revised in the future. Despite the challenges of working with incomplete information to try to create a world view of how larger mind features, there are some main potential rewards. It is type of certain that an incomplete anatomic model is best than no actual mannequin. Knowing that the operate is grossly situated within the lateral frontal lobe may go in research, but millimeterscount in surgery. The goal of this chapter is to provide a complicated anatomic framework of the gross cerebral anatomy underlying specific higher mind functions from which to base any further discussion on tips on how to protect cerebral features in surgery. This article is the first that I know of to attempt to demonstrate the anatomy of higher brain functions in a surgically and anatomically useful framework, and hopefully, it will be the start of a long future of critically revising and refining these models. We have grounded all of our work with connectomics in the Human Connectome Parcellation scheme. Examples of the parcellations can be seen in the figures in Chapter 3; however, completely describing these areas is beyond the scope of this e-book and would require a book of its own. With the thought that these models are aimed toward clinically useable as opposed to comprehensive maps of brain perform, I went about making these maps within the following manner: 1. We utilized neuropsychologic and practical imaging literature paired with my very own experiences with awake mind surgery to create a primary concept about what the networks ought to roughly entail. We performed coordinate meta-analysis to decide statistical areas of activation in a standardized coordinate area. We then utilized tractography to identify which fibers, if any, joined these areas. It is for certain that the creation of higher human abilities involve interactions between networks. For example, interactions between visible, semantic, and face motor methods are essential to name objects. The bidirectional communication between these two cortices is putting, 3) in the third set of panels, we add the premotor cortex in pink. The curved medial bend of the fibers into the descending motor fibers could be visualized bending into the page to run across the insula, 2) the second set of panels demonstrate the addition of the sensory cortex communications in darkish blue. The bilateral communication between these two cortices is striking, 3) in the third set of panels, we add the premotor cortex in pink. The model is steadily inbuilt these sequential pictures in a sequential method in order that the relative contributions of every element could be distinguished. The yellow fibers highlighted reveal communication between the premotor cortices and the basal ganglia. It is probable that nearly all core neurofunctional units of the cerebrum must access the motor system at some point to make a clinically observable output, however oblique which could be. This is logical given its key function in coordinating advanced coordinate actions corresponding to alternating finger actions, which would not be wanted in lower animals which hemibody movements could suffice. Third, restoration most likely entails the contralateral motor system taking over, and chopping the corpus callosum fibers can prevent restoration from taking place (see Chapter 17). In addition to its well-known function in organizing motor signals to be sent to downstream effectors such as the motor cortex, a typical means it interacts with other methods is as a decide which compares and assesses information deciding the relative importance of various streams of data. Basal Ganglia the putamen, globus pallidus, subthalamic nucleus and substantia nigra are well-known to all as key components of the motor system. Somatosensory Cortices For years, I was underneath the impression that the goal of brain mapping and finding the sensory strip, was to have a transparent concept where the motor strip was. It was greatest, obviously, to avoid the sensory cortex, however at worse the problem can be a numb leg and/or hand. I suspect many still assume in these phrases today, although if asked on the boards no one would counsel this could be a good thought out loud. This truth highlights a key flaw in our considering that may solely be exposed by careful thought given to the study of brain connectivity. Superior Parietal Lobule and Banks of the Intraparietal Sulcus As described below, greater level visible processing has typically been described as flowing out from the occipital lobe in two basic streams: the Ventral "what" pathway and the Dorsal "where" pathway. The dorsal stream ("where") is progressively processed in the precuneus and neighboring occipital lobe earlier than sending its output to the superior and inferior parietal lobules. Because the direct input from the visual system to the motor system is at greatest limited, the superior parietal lobule probably is involved in integrating visible, proprioceptive, and somatosensory inputs and feeding this data ahead to the motor system the place it helps shape movements. Numerous studies have particularly linked the intraparietal sulcus and its banks to maps of private and extrapersonal house, and their roles in visible steerage shaping of hand actions to conform to targets throughout reaching, grasping and manipulation. The position of the intraparietal sulcus and its banks, which in likelihood is the place our spatiotemporal maps of the world are stored, ought to give us pause earlier than selecting this sulcus as a path to the atrium of the lateral ventricle. While this may seemingly assist the Duffau or Mesulam mannequin, it is important to notice that these connections are nearly completely to areas V1-4, that are very early visual areas, suggesting that the relationship is a little more advanced than merely visual to semantic switch.
Alavert 10 mg order
The location of the interior iliac vessels is often ascertained during gynecologic surgical procedure allergy symptoms loss of taste discount alavert 10 mg otc. The uterine artery arises from the anterior division of the inner iliac artery allergy forecast kitchener alavert 10 mg order with visa. The incidence of retroaortic and circumaortic left renal vein is roughly 7%2 and ought to be acknowledged when one is performing nodal dissection within the aortocaval window, to avoid injury. The uterine veins typically drain into their respective internal iliac veins, which then be part of the respective exterior iliac veins to kind the widespread iliac veins. The potential for important bleeding during pelvic surgical procedures is properly acknowledged. Such bleeding could occur, in part, because of the concentration of the major vessels and the intricate venous plexus. Deliberate ligation (or clipping) and division of crossing venous tributaries in the pelvis assist avoid vessel tearing and prevent excessive bleeding. There is a rich collateral community between the best and left inside iliac arteries and veins, respectively. Similar anastomotic connections exist between the inferior mesenteric vein, which often joins the splenoportal system, and center rectal vein, which drains into the internal iliac vein. Hence ligation of the internal iliac artery or vein, or their respective branches and tributaries, is mostly nicely tolerated with out scientific penalties. However, when attainable, the authors suggest preservation of flow to a minimal of one internal iliac artery, to keep away from the rare however probably disabling prevalence of pelvic ischemia. Arteries and veins of the pelvis, conventionally given the identical names, are shown running facet by side. Intraoperative images of a left inguinal metastatic mass involving the frequent femoral vein and artery. Major harm to the common iliac, external iliac, common femoral, and superficial femoral arteries requires vessel restore or reconstruction to keep decrease limb perfusion. The profunda femoral artery can usually be sacrificed without causing limb ischemia as lengthy as the superficial femoral artery is preserved. The frequent femoral and iliac veins are the principle venous drainage for the lower extremity, and acute ligation of those vessels will generally lead to extreme ipsilateral leg swelling. Occasionally, ligation of the external iliac vein might not cause extreme postoperative limb swelling, if it had been chronically occluded and if venous drainage is maintained via collaterals. These tributaries can function collaterals between the leg and the belly wall venous plexuses within the presence of central venous obstruction involving the external or common iliac veins. Preservation of the exterior iliac and customary femoral veins is beneficial to forestall severe limb swelling. However, these can be ligated when massive hemorrhage is encountered throughout troublesome surgical dissection as a lifesaving measure. Gynecologic Malignancy Involving Major Vessels At occasions, gynecologic cancers can abut, invade, or encase major blood vessels. Decisions concerning operative Chapter 22 Management of Vascular Complications 305 administration should involve the consideration of a quantity of key factors related to each the tumor and the particular vessels concerned. Relevant elements to consider include the extent of the illness, plans for any adjuvant remedy, and the biological responsiveness of the tumor to different therapy modalities. In addition, one should additionally think about whether the patient has other recognized sites of residual illness. In these complicated circumstances, careful preoperative planning and collaboration between the first gynecologic oncology surgeon and a vascular surgeon are paramount for a successful affected person end result. The choice making must be custom-made to the individual patient, primarily based on the type and extent of the malignancy being treated and the significance of the vascular construction concerned. Improvement in radiologic imaging has contributed to the advances made in most cancers staging and therapy end result. Selective catheter-based angiography is now reserved primarily for planned therapeutic endovascular interventions. Contraindications to iodinated contrast infusion include severe renal insufficiency and history of allergy (anaphylactic reaction) to iodinated distinction. B-mode vascular ultrasonography offers a two-dimensional image of the vessel wall and lumen. Color move imaging and pulsed Doppler waveform analysis provide a real-time evaluation of blood move characteristics. In addition, venous duplex ultrasonography could also be used preoperatively to map out potential venous conduits (such as the nice saphenous, femoral, or inside jugular veins) and procure info concerning location, quality, diameter, length, and depth. Similarly, arterial duplex ultrasonography can provide invaluable assessment of the arterial patency and the presence and placement of arterial disease in the lower extremities. Vascular duplex ultrasonography is a practical imaging modality that could be carried out within the outpatient clinic or at the bedside. Acute Major Intraoperative Vascular Injuries Complications during gynecologic procedures performed with laparoscopic, robotic, or open surgical techniques are uncommon. However, damage to the most important blood vessels in the abdomen and pelvis may be life-threatening. Fortunately, the incidence of inadvertent major intraabdominal vessel injury is less than 1 per 1000 instances. The danger of vascular harm is increased in sufferers with pelvic malignancy, partially as a end result of the bulky tumor mass can distort the encircling anatomy, making surgical dissection harder. In addition, neoadjuvant treatments-in particular, radiation therapy-can lead to the effacement of the tissue planes across the vessels. The Chapter 22 Management of Vascular Complications 307 following section describes operative maneuvers to prevent or control main bleeding which are obtainable to the gynecologic oncology surgeon. Prevention of Vascular Injuries Vascular injuries can happen as entrance accidents during the placement of trocars in a laparoscopic or robotic procedure. Injury also can occur in the course of the dissection of perivascular nodal tissue or the dissection of a tumor lying towards a major vessel throughout a laparoscopic, robotic, or open process. The optimal methodology for coping with vascular injuries is to be aware that these can happen at any time and to never assume immunity towards them. Best outcomes are usually the results of meticulous evaluation of the anatomy and body habitus of the affected person and, in oncologic procedures, the research of the anatomy of the tumor and its relation to the encircling buildings. In oncologic procedures, the larger the burden of the tumor or nodal illness, the higher the risk of inadvertent vascular accidents. High-risk procedures that will require a vascular intervention ought to ideally be accomplished early within the day, when the weather of each experience and good scientific acumen are at their best. However, the preemptive deployment of an endovascular stent earlier than removing of tumor stays anecdotal, and extra research are wanted to justify this system. Dissection of the tumor (asterisk) in the left pelvis removed a half of the anterior wall of the frequent iliac artery (A). No bleeding was encountered in this patient because a covered stent (arrow) was current within the artery. Principles of Vascular Repair A main vascular damage is an emergency, and the best action to management the bleeding is quick direct strain on the bleeding point and a name for assistance with out hesitation.
Purchase alavert 10 mg otc
The cardinal ligaments are condensations of connective tissue which might be a number of centimeters in width and run from the cervix and upper vagina to the pelvic sidewall allergy symptoms of gluten alavert 10 mg safe. The uterosacral ligaments are bands of connective tissue that are attached with the cardinal ligaments at their level of insertion within the cervix and upper vagina allergy shots years discount 10 mg alavert with mastercard. The uterosacral ligaments cross posteriorly and inferiorly to attach to the ischial spine and sacrum. The parametrium may be artificially divided into three bands of connective tissue: the posterior parametrium or uterosacral ligament, the cardinal ligament or lateral parametrium, and the cervicovesical ligament or anterior parametrium. The uterosacral ligaments are bands of connective tissue joining the cardinal ligaments at their point of insertion in the cervix. The uterosacral ligaments move posteriorly and inferiorly to attain the ischial spine and sacrum. This ligament lies in close contact with the ureter before crossing the uterine artery throughout the lateral parametrium. The hypogastric nerve runs 1 to 2 cm inferior to the ureter and alongside the lateral facet of the uterosacral ligament. The lateral parametrium contains the uterine artery and veins (superficial and deep) and a few variable number of parametrial lymph nodes; in its deepest portion-close to the pelvic floor-appear the parasympathetic nerves (splanchnic nerves) coming from roots S2 to S4. Uterine Support Structures the buildings that join the cervix and vagina to the pelvic sidewall and sacrum are known as the cardinal and uterosacral ligaments, respectively or in conjunction, uterine parametria. They originate on the uterine fundus anteriorly and inferiorly to the fallopian tubes, run retroperitoneally through the broad ligament, after which enter the inguinal canal, terminating within the labia majora. Parametria the cardinal-uterosacral ligament complex suspends the uterus and higher vagina in their regular place. It serves to Broad Ligament the broad ligament covers the lateral uterine corpus and higher cervix. The anterior parametrium is also called the bladder pillar or vesicouterine ligament. The pelvic splanchnic nerves are parasympathetic nerves coursing in the lower side of the lateral parametrium. The efferent nerves of the inferior hypogastric plexus course alongside the lower aspect of the anterior parametrium. It consists of anterior and posterior leaves that separate to enclose viscera and blood vessels. Dissection between these sheets is necessary to present retroperitoneal exposure of those buildings. Various zones of the broad ligament are named for close by structures such because the mesosalpinx (located near the fallopian tubes) and the mesovarium (located close to the ovary). The broad ligament consists of visceral and parietal peritoneum that accommodates clean muscle and connective tissue. Pelvic Vasculature Arterial Supply the aorta supplies the blood supply to the pelvic buildings. The aorta bifurcates at approximately the level of L4 to L5 into the right and left frequent iliac arteries. The frequent iliac arteries divide into the exterior iliac and inner iliac arteries; the inner iliac artery can be referred to because the hypogastric artery and supplies a lot of the vascularization to the pelvic viscera and pelvic facet wall and the gluteal muscles. The left frequent iliac vein travels anterior to the sacrum and medial to the aortic bifurcation and joins the best frequent iliac vein to kind the vena cava beneath the right widespread iliac artery. The external iliac artery is situated medial to the psoas muscle; it continues its course caudally to in the end give off the femoral artery after crossing beneath the inguinal ligament. In the pelvis, the exterior iliac artery has few branches; these include the inferior epigastric artery and a variable superior vesical artery. The exterior iliac vein is far larger and lies posterior and medial to the artery. The exterior iliac vein additionally passes beneath the inguinal ligament earlier than reaching the thigh. The inferior epigastric artery originates from the exterior iliac artery and travels via the transversalis fascia into a space between the rectus muscle and posterior sheath. In their course from the lateral position of the external iliac vessels, the inferior epigastric artery and vein run obliquely toward a extra medial location as they approach the umbilicus. The superficial epigastric vessels originate from the femoral artery, perfuse the anterior belly wall, and branch extensively as they strategy the umbilicus. The posterior division runs toward the big sciatic notch, dividing into the lateral sacral, iliolumbar, and superior gluteal arteries. The anterior division of the interior iliac artery branches into the obliterated umbilical, uterine, superior vesical, obturator, vaginal, and inferior gluteal and internal pudendal arteries. To attain the perineum, the internal pudendal artery courses via the higher sciatic foramen, across the sacrospinous ligament, and again in by way of the lesser sciatic foramen. Its branches provide the anal sphincter, the pelvic diaphragm, and the external genital constructions within the feminine. The inside iliac artery is a retroperitoneal construction; for any of its branches to be identified and accessed, Ascending branch Anastomosis External iliac a. Superior hypogastric plexus External iliac Common iliac Anterior division Posterior division Lumbar Iliac Iliolumbar Obliterated umbilical Superior vesical Vesicle Ureteric Vasal Obturator foramen Inferior vesical Ureteric Vesicle To lig. The most fixed arteries are superior vesical, uterine, internal pudendal, inferior gluteal, and superior gluteal. Chapter 2 Abdominal and Pelvic Anatomy 13 a retroperitoneal dissection have to be performed. Most of the blood provide to the uterus, tubes, and ovaries derives from the uterine and ovarian arteries. The uterine arteries originate from the anterior division of the inner iliac arteries within the retroperitoneum. They normally share a typical origin with the obliterated umbilical artery or superior vesical artery. The obliterated umbilical arteries, also referred to as superior vesical arteries and as lateral umbilical ligaments, are a helpful landmark for the identification of the uterine artery. Simply pulling up the obliterated umbilical artery permits straightforward identification of the uterine artery. The uterine artery travels by way of the cardinal ligament over the ureter and approximately 1. It then joins the uterus near the level of the inner cervical os, branching upward and downward toward the uterine corpus and inferiorly towards the cervix. The uterine corpus branches anastomose with vessels that derive from the ovarian arteries, thus offering collateral blood flow. The uterine artery additionally sends a branch to the cervicovaginal confluence at the lateral aspect of the vagina. The vagina additionally receives its blood provide from this uterine department, in addition to from a vaginal branch of the interior iliac artery, which anastomoses alongside the lateral wall of the vagina. The ovarian vessels journey by way of the infundibulopelvic ligaments in proximity to the ureter, along the medial aspect of the psoas muscle. The ureter is supplied by small branches of the blood vessels it crosses: the widespread iliac, internal iliac, and superior and inferior vesical arteries.
Buy cheap alavert 10 mg on line
A median of sixteen pelvic nodes (range allergy testing evansville in order alavert 10 mg amex, 1�31 nodes) and seven paraaortic nodes (range allergy testing pediatrics discount alavert 10 mg with mastercard, 2�28 nodes) have been retrieved. The median operative time and estimated blood loss had been 129 minutes (range, 45�321 minutes) and 70 mL (range, 10�500 mL). Conversion to laparotomy was essential in one woman to restore an obturator nerve injured during pelvic lymphadenectomy. Median operative time and estimated blood loss have been 260 minutes (range, 149�380 minutes) and 60 mL (range, 25�350 mL). Laparotomy was carried out in a second girl for repair of an external iliac vein damage that occurred throughout lymphadenectomy. No recurrences have been noted throughout restricted follow-up (median, eleven months; range, 1�35 months). Although these appear believable and will make intuitive sense, their confirmation requires further examine with the efficiency of additional, larger, randomized controlled trials. Postoperative Pain Postoperative ache after gynecologic surgical procedures varies and is affected by each patient and technical elements, each modifiable and unmodifiable. No differences in operative time, estimated blood loss, length of stay, or complication rate had been noted between the groups. This extended analysis was possible due to the culture of longer hospitalization (length of stay >3 days for both groups) in the nation where the examine was performed (Taiwan). Neither postoperative pain 12 hours after operation nor shoulder ache at any time level differed between surgical approaches. This lack of blinding with respect to surgical approach may conceivably have influenced the outcomes. The anesthesiology protocol, including administration of ache drugs intraoperatively, was strictly standardized. Of note, no preoperative or postoperative local anesthesia was used at skin incisions. No intraoperative problems or conversions to laparotomy occurred in either group, and operative times were similar. The difference was greatest and statistically significant at 4 hours postoperatively (P =. No distinction in ache was reported between surgical approaches on the time of discharge (mean hospital stay of 1. Thus, although the measured differences in postoperative pain and analgesia use achieved statistical significance, their clinical significance could also be debated. Both total postoperative pain and shoulder-specific postoperative ache were assessed at 6 and 24 hours after operation by using a 10-point scale. Women in both teams reported related ranges of ache at 6 and 24 hours after operation (2. The impact of the rigorous preoperative analgesia protocol as well as local anesthetic injections on these outcomes is unclear however might have contributed to improved pain measures across surgical approaches. Detailed info concerning fascial closure methodology and follow-up evaluation was not reported in several research. Of note, there have been no significant differences between the two groups with regard to medical demographic information, operative times, uterine weights, perioperative complication fee, postoperative hospital stay, postoperative ache scores, or analgesic use. In a survey examine, 250 women were proven a sequence of photographs of an unscarred female stomach. Previous studies have demonstrated a correlation between trocar measurement and risk of incisional hernia, lending validity to this concern. After extension of an incision and mass extraction, efficiency of moreover indicated procedures may be challenging owing to problem with upkeep of pneumoperitoneum. This facilitates correct thorough intraperitoneal analysis during complete surgical staging of gynecologic malignancies while minimizing potential incisional morbidity. Challenges of Laparoendoscopic Single-Site Surgery Initial growth of laparoscopy entailed use of a single incision and a laparoscope that included a channel for passage of one easy software corresponding to biopsy forceps. Ongoing advances in instrumentation are actually providing completely different options to these technical challenges and encourage reconsideration of the usage of a single incision for laparoscopic surgical procedure. Maintenance of Pneumoperitoneum Pneumoperitoneum is crucial for performance of laparoscopy and requires an airtight seal between laparoscopic ports and the body wall. A variety of industry-developed entry gadgets are available that overcome this problem. Each design has strengths as nicely as limitations, which can or may not be pertinent relying on the needs of the surgeon and the particular case. An introducer is used to place one ring by way of a small incision into the peritoneal cavity. The second ring is pushed flush to the skin of the abdomen because the intervening plastic sleeve is pulled tight. The design with respect to the cap differs in terms of number3�5 and size (5�15 mm) of available port openings. The openings are flexible and allow placement of both straight or curved devices. The wound retractor consists of two versatile plastic rings with an intervening sleeve. The other ring is pulled tight to the skin by decreasing the size of the intervening plastic sleeve. Once the apparatus is tightly in place on the abdominal wall, a removable GelSeal cap is utilized. Three 5- to 10-mm and one 12-mm selfretaining low-profile sleeves (ports) are included and can be placed through the gel in any desirable configuration. It is positioned inside an incision and meant to span the physique wall however is at present obtainable in just one size (approximately 4 cm in length). Individual ports 5 to 15 mm in diameter are then positioned through three of the channels. Multiple low-profile ports could be positioned through separate fascial punctures in a single skin incision. One artistic solution for upkeep of a pneumoperitoneum with passage of a number of devices is the usage of a surgical glove applied over an Alexis Wound Retractor (Applied Medical). The design of some port techniques allows for individual ports inside the identical incision to be located farther from one another outdoors the physique. Regardless, they have to all move via a single fascial defect, the size of which limits the benefit of prolonged port spacing. Staggering the length of instruments in order that hands are spaced away from each other vertically may be of assistance. A wide number of disposable and a limited choice of reusable articulating instruments, including graspers, needle drivers, scissors, staplers, and suturing and vitality gadgets, are at present out there. The instruments are positioned through a port whereas straight after which actuated to bend up to ninety levels. Although reusable fixed-curved instruments can be found (Olympus America), they can be utilized solely with access gadgets that use very brief port lengths. The AnchorPort Single Incision Laparoscopy Kit (SurgiQuest, Milford, Connecticut) contains three specialised 5-mm ports that "self-anchor" to the abdominal wall and "self-adjust" to the thickness of the wall. The self-adjusting design minimizes the area occupied by the port each inside and outside the incision, permitting the ports to be positioned in close proximity to each other.
Diseases
- Thanos Stewart Zonana syndrome
- Hallervorden Spatz disease
- Warfarin antenatal infection
- Chromosome 6, monosomy 6p23
- Congenital spherocytic anemia
- Cole carpenter syndrome
- Duplication of the thumb unilateral biphalangeal
- Hypocalcinuric hypercalcemia, familial type 1
- Acral renal mandibular syndrome
Purchase alavert 10 mg overnight delivery
Furthermore allergy shots immune system alavert 10 mg order free shipping, sufferers whose cytoreduction entails splenectomy extra commonly require diaphragm peritonectomy and radical pelvic surgery allergy forecast arlington va buy 10 mg alavert otc. In the presence of illness, the splenic hilum is mostly concerned, followed by the surface of the spleen, and finally the parenchyma. In addition to resection at main operation, isolated splenic metastases may be seen in patients with recurrent illness. Spleen Exposure As previously described, publicity of the upper abdomen relies on an appropriate incision and use of a self-retaining retractor. For entry to the spleen, the left costal margin is retracted superiorly and laterally. This will assist information the surgical plan, dictating whether a piecemeal or en bloc resection shall be required. This illness distribution precludes the anterior method, and the operating surgeon should be comfy approaching splenectomy posteriorly. Initially the abdomen is decompressed by means of an oral gastric or nasogastric tube positioned on low continuous suction. The decompressed stomach is then placed on medial traction through the use of a Babcock clamp. Attachments between the spleen and the anterior stomach wall and left diaphragm are taken down with Chapter 12 Radical Upper Abdominal Surgery: Liver, Diaphragm, and Spleen 169 electrosurgical energy and blunt dissection. This dissection then permits for mobilization of the spleen superiorly and medially, bringing it into the operative field. At this level the splenorenal (or lienorenal) ligament is incised, liberating the spleen from the left kidney. Further rotation of the specimen then permits for posterior palpation of the splenic vessels. It is essential to notice that in as a lot as 75% of circumstances, the tail of the pancreas lies inside 1 cm of the splenic hilum and should be mobilized sufficiently to keep away from damage because the splenic vessels are secured. The splenic artery ought to be ligated primarily, allowing for autotransfusion and splenic decompression earlier than the splenic vein is ligated and transected. The artery and vein should be divided individually to avoid arteriovenous fistula formation. After the primary vessels have been secured, the specimen is rotated additional within the medial path and the remainder of the gastrosplenic ligament, inclusive of the short gastric vessels, is cauterized and transected with a bipolar vascular sealing device. As detailed earlier, the splenic flexure is mobilized primarily, and the splenocolic ligament is then incised with a laparoscopic vascular sealing system. The lateral splenic attachments (splenophrenic and splenorenal ligaments) are then incised, permitting for improved medial mobilization of the spleen. The dissection is directed medially, with coagulation and transection of the short gastric vessels as they course through the gastrosplenic ligament. The splenic artery and vein are recognized and secured with a laparoscopic vascular stapling device. Splenic Injury the most common indication for iatrogenic splenectomy is splenic laceration because of traction at the time of omentectomy. Excessive traction can lead to vascular harm or splenic capsule trauma and bleeding. Attempts at conservative management may be made with topical hemostatic brokers corresponding to Surgicel or Fibrillar (Ethicon Inc. The use of an omental pedicle to tamponade the surface bleeding has also been described. Ultimately, within the occasion of a major floor damage or hilar injury, conservative measures ought to be deserted and a splenectomy performed. Distal Pancreatectomy the tail of the pancreas is intimately associated with the splenic hilum. In some cases the presence of metastatic illness involving the tail of the pancreas might necessitate a distal pancreatectomy. In prior series, the frequency of distal pancreatectomy was reported to be as high as 11% at the time of surgical cytoreduction. The distal pancreatectomy is performed as a continuation of the splenic dissection as outlined earlier. The posterior peritoneal reflection of the pancreas is identified and blunt dissection used, permitting for elevation of the tail of the pancreas with the primary specimen. It is important to perceive the anatomic location of the splenic vein posterior to the physique of the pancreas and to additionally anticipate drainage of the inferior mesenteric vein into the splenic vein. Once elevated, the resection line and extent of distal pancreatectomy are governed by tumor distribution and need for complete gross resection. When the bipolar system is used, the resection margin can be strengthened with a 2-0 silk or alternate delayed absorbable suture. Anterior Approach If the anterior floor of the spleen is freed from illness, the anterior approach affords the most direct path to secure the splenic vascular provide. As a half of the omentectomy, the gastrocolic ligament is incised and the left gastroduodenal vessels are cauterized and transected. This facilitates entry into the lesser sac, and the body and tail of the pancreas could be identified along the ground of the lesser sac. Medial traction is once again used on the decompressed abdomen, and the inferior facet of the gastrosplenic ligament is taken down by using the vascular sealing gadget or laparoscopic stapler. The splenic artery can then be recognized coursing instantly superior to the pancreas. The peritoneum overlying the pancreas is rigorously incised, and the splenic artery is skeletonized with a proper angle clamp, secured via ligatures, and transected. After the splenic artery has been secured, autotransfusion happens, and any remaining quick gastric vessels could be secured by way of the vessel sealing device. The spleen can then be rotated medially and superiorly, and the lateral attachments taken down in a fashion analogous to that employed in the posterior approach. Laparoscopic Splenectomy In cases of isolated splenic recurrence, a minimally invasive approach can be utilized to lower operative morbidity and allow for extra rapid restoration and initiation of chemotherapy. This process must be reserved for instances by which the surgical end result is anticipated to be no gross residual illness. Such contiguous lesions might involve the transverse colon, omentum, greater curvature of the stomach, left diaphragm, distal pancreas, and spleen. Before committing to such an intensive resection, one ought to conduct a comprehensive assessment to guarantee feasibility and confirm that reestablishing intestinal continuity after cytoreduction is feasible. Although radical in nature, this procedure primarily combines the principles beforehand reviewed on this chapter. The falciform, left coronary, and left triangular ligaments are incised sequentially, permitting for medial mobilization of the left lobe of the liver.
Alavert 10 mg buy without prescription
Proximal and distal bowel clamps are beneficial to minimize spillage of intestinal contents allergy symptoms to beer buy generic alavert 10 mg online. An incision is created on the antimesenteric border of the large-caliber bowel segment allergy katy tx 10 mg alavert purchase amex. The anastomosis is accomplished using a one- or two-layered hand-sewn technique Small Bowel Resection the particular strategy of small bowel resection will range based on the medical situation, however normally, it could be damaged down into 5 primary elements: 1. This ensures that the planned resection will accomplish its intended purpose and that the anastomosis shall be technically possible, well perfused, and viable. The segment of the small bowel to be eliminated ought to be clearly demarcated at the proximal and distal factors, leaving approximately 5-cm segments of healthy bowel on both aspect to guarantee an enough margin of resection. Holding sutures are positioned across the circumference of both intestinal lumina, one suture securing together the antimesenteric borders of each intestinal segments. The linear anastomotic stapler is positioned into the lumina, secured and locked in place, and fired. To prevent spillage of bowel contents immediately into the abdominal cavity, warm moist lap packs can be utilized to isolate the specimen, and soft bowel clamps may be applied about 20 cm from the proximal and distal bowel finish to avoid extra contamination. Mesenterectomies are created by way of home windows of Deaver on the corresponding proximal and distal factors of resection. Whether a linear stapler or traditional clamps are used, transecting the bowel at an oblique angle in a trend such that the larger portion is removed from the antimesenteric side ensures adequate vascular perfusion to the entire transected edge. The antimesenteric aspect of the bowel is the realm farthest away from the mesenteric perfusion, and trimming the antimesenteric end obliquely permits for enough perfusion. If this is the case, the distal ileum must be included in the resection and the anastomosis performed to the cecum or ascending colon. Ileocecal Resection Tumor involvement of the ileocecal area or a bowel obstruction of the terminal ileum can mandate resection of the terminal ileum in conjunction with a portion of the ascending colon. The tumor-involved intestine is mobilized by incising the parietal peritoneum from the terminal ileum, across the cecum, and along the white line of Toldt up to the hepatic flexure. The ileum is then mobilized by incising along the bottom of the small bowel mesentery towards the ligament of Treitz. The terminal ileum, ascending colon, and proximal transverse colon are reflected medially, taking care to not injure the proper ureter, ovarian vessels, duodenum, and head of the pancreas. As beforehand talked about, the distal eight to 10 cm of ileum must be removed with the cecum, because this space can have an inconsistent blood supply, which may lead to a poorly vascularized anastomosis. The mesentery can be divided as beforehand described and the vascular pedicles secured utilizing conventional clamps and ties or a vessel sealer (LigaSure) before removal of the specimen en bloc. A side-to-side (functional end-to-end) ileo�ascending colon anastomosis offers for a extensively patent lumen and is the method of alternative for reestablishing intestinal continuity. Either a hand-sewn or a stapled technique is applicable; nevertheless, stapled anastomosis may be related to fewer leaks than the hand-sewn ileocolic anastomosis. Patients who endure an ileocecal resection may experience extra frequent bowel movements and watery bowel actions on account of the lack of the ileocecal valve. This may be associated with nausea because of reflux of colonic contents into the small bowel. Bowel operate may improve with time, however sufferers have to pay attention to preliminary changes of bowel function after ileocecal resection and possible long-term adjustments in bowel perform. In choose situations, end-to-end or end-to-side anastomosis, as previously described, may be applicable. Left Hemicolectomy in Conjunction With Omental Disease the descending colon is retracted medially after incising along the white line of Toldt, and the splenic flexure is mobilized by dividing the phrenocolic and lienocolic ligaments. Care have to be taken throughout splenic flexure mobilization to avoid extreme downward traction, which may result in capsular tear to the spleen. The middle colic artery ought to be identified and preserved; however, the left-sided branch may be integrated inside the scope of the resection. The anastomosis can be accomplished by the use of considered one of several strategies with a stapled or hand-sewn closure. Rectal Resection Rectal resection is usually performed by gynecologic oncologists within the setting of pelvic illness involving the pelvic peritoneum with sigmoid colon and/or rectum. The surgical resection of all or part of the rectum with a primary anastomosis is termed a low anterior resection. Most frequent indications are in patients with superior ovarian most cancers requiring a rectal resection as part of the debulking surgery, normally within the setting of an en bloc resection with uterus, cervix, higher vagina, and adnexa. Other indications embrace locally advanced endometrial most cancers or cervical cancer or recurrent most cancers surgical procedure. The threat of anastomotic leak is biggest in rectal surgery as a outcome of the perfusion could additionally be compromised, and guaranteeing a tension-free anastomosis is extra difficult than within the proximal a part of the colon. Key parts of a profitable rectal resection are the integrity of the rectal wall distal to the anastomosis, enough perfusion both proximal and distal to the anastomosis, and the absence of pressure proximal to the anastomosis. In basic, the closer the anastomosis to the anal verge, the higher the chance of anastomotic leak. The most typical causes for an anastomotic leak include compromised perfusion and pressure as well as injury to the distal rectal wall throughout preparation for anastomosis, leading to poor perfusion and necrosis. Developing the correct surgical planes, maintaining the integrity of the rectal wall throughout dissection of the mesorectum, and mobilizing the proximal colon rigorously and completely are key elements of a profitable rectal resection and anastomosis. When carried out for rectal most cancers, the operation features a complete mesorectal excision with an anastomosis on the stage of the pelvic floor. For gynecologic cancers, the dissection stays outdoors the fascia propria and closer to the pelvic aspect walls to include the pelvic illness. Gynecologic cancers often grow above the peritoneal reflection, and very deep resections past the peritoneal reflection are unusual. In general, a partial mesorectal excision with a 5- to 7-cm distal and mesorectal margin is commonly adequate. Once beyond the peritoneal Transverse Colectomy the transverse colon and its mesentery could additionally be immediately infiltrated by bulky omental disease, or the associated fibrotic inflammatory tissue reaction could make separation along anatomic planes difficult. The omentum is divided from the lateral aspects of the transverse colon, and the lesser sac is entered. The transverse colon is then fully mobilized by dividing the gastrocolic ligament from the higher curvature of the stomach and taking down the lineocolic ligaments to free the hepatic flexure and splenic flexure, respectively. The surgeon should be sure that the marginal artery of Drummond is intact and will present adequate blood provide to each ends of the deliberate anastomosis. If the marginal artery of Drummond is found to be discontinuous at the splenic flexure, the distal transverse colon and proximal descending colon are included in the scope of the resection. A colocolostomy is created to reestablish continuity by way of both an end-to-end or a practical end-to-end stapled or hand-sewn anastomosis. Right Hemicolectomy in Conjunction With Omental Disease Extensive omental tumor involving the ascending colon or hepatic flexure warrants an en bloc proper hemicolectomy. The terminal ileum, cecum, and ascending colon, together with the hepatic flexure, ought to be mobilized. The right colon is elevated off of the retroperitoneum by rigorously releasing the mesentery from the underlying kidney, ureter, ovarian vessels, and inferior vena cava. In most circumstances, the right-sided department of the middle colic artery may even have to be sacrificed, but the center colic artery ought to be preserved. The anastomosis can be completed with one of a quantity of methods through the use of a stapled or hand-sewn closure.
10 mg alavert order mastercard
If the injury occurs deeper into the pelvis allergy vs adverse drug reaction alavert 10 mg generic without prescription, on the distal one-third of the ureter allergy medicine for asthma 10 mg alavert with mastercard, then reimplantation into the bladder as a ureteroneocystostomy is most well-liked and is completed with use of bladder mobilization and a Boari flap or psoas hitch repair. In distinction, aberrant colonic blood provide occurs more incessantly, and figuring out variations proves essential to guaranteeing sufficient supply to any anastomosis. Often, these branches can be originating collectively at one massive frequent trunk, making their dissection, identification, and management difficult. This normal anatomy may be confusing without proper identification, resulting in frustratingly significant hemorrhage if not identified appropriately earlier than harm happens. Given that normal anatomy occurs less incessantly than beforehand described, data of aberrant vasculature is key to correct dissection and avoidance of inadvertent injury that may result in vessel ligation or inadequate tissue perfusion and subsequent ischemia. Methods include palpation of the terminal arcade, such as the marginal artery for the colon, Doppler ultrasound of vessels to ensure arterial pulsatile flow, and use of fluorescence with a Wood lamp to affirm tissue perfusion. If this flow is confirmed, sufficient blood provide has been confirmed for an anastomosis to heal. If lower than pulsatile bleeding is encountered, more proximal transection must be considered to guarantee enough blood flow; as a precept in bowel surgery, this should all the time be followed. Vascular Hemorrhage Advancements in surgical vitality devices have expedited surgical procedures. Although these vitality units may be costly, they seal and ligate vessels 7 mm or less in diameter and scale back operative time and hemorrhage. These units may also be used during conventional open operations, however the authors favor a standard vascular ligation between clamps with suture ligature and ties. Preoperative evaluate of the major vasculature is paramount to understanding vascular anatomy and relationships with adjacent constructions. Dissection of main vessels may be treacherous, especially during a repeat abdominopelvic operation or after pelvic radiation. If unanticipated hemorrhage is encountered, the fundamental principle of vascular surgery have to be followed, gaining each proximal and distal control to properly identify the harm and not cause additional harm (see Chapter 22). This is critical when dissecting alongside the aorta, its anterior visceral branches, lateral renal branches, and pelvic vessels branching off the widespread iliac artery and veins. This is especially necessary when working in the lateral pelvis, and an open approach is almost always essential to control the bleeding that may develop with injury to these vessels. Exposure is a key think about addressing vascular hemorrhage; incisions ought to permit for maximum entry, or poor visualization will prolong restore. Vessel loops are sometimes used to encircle the vessels on both the proximal and the distal sides of damage as quickly as circumferentially dissected to acquire control with out inflicting further vascular injury. It is equally necessary to notify anesthesia suppliers when main bleeding is encountered, and intermittent direct stress may be necessary to permit the anesthesia team to meet up with their resuscitation. Simple restore of those buildings requires use of 4-0 or 5-0 monofilament permanent suture; nevertheless, if luminal compromise is a concern, a patch angioplasty with saphenous vein or bovine pericardium can be utilized, though usually this is carried out by a vascular surgeon. Additional bleeding can come from smaller bridging vessels that course alongside the inner iliac vessels. When bleeding is recognized, use of simple monopolar cautery is usually inadequate to control it, but use of a bipolar power system will normally provide enough management. Standard clamp and tie strategies are additionally enough however can require a for a lot longer time. A return trip to the working room could be planned and extra assistance used as needed throughout the 24 to forty eight hours after stabilization. Many advances have occurred because the description of the first diagnostic laparoscopy, performed by Raoul Palmer, was revealed in 1947. The most popular entry methods could be broadly categorised as open or closed, and essentially the most commonly chosen entry web site is the umbilicus. A Cochrane evaluate examined the risks of visceral and vascular injury between the two methods and located no benefit to both approach. The open approach, or Hasson approach, includes making a 10-mm infraumbilical incision, isolating the umbilical stump, and dissecting the subcutaneous tissue away from the anterior stomach wall. The umbilical stump is lifted away from the stomach, and the linea alba is incised to reveal the peritoneum. The peritoneum is entered underneath direct visualization, and for this reason this method is chosen typically in patients with earlier belly surgery. The closed-entry technique uses an analogous strategy to figuring out the umbilical stump; however, as a substitute of incision of the linea alba, a Veress needle is inserted into the stomach to establish pneumoperitoneum. Once this has been achieved, a trocar is inserted into the abdomen, and the abdominal contents are examined. However, the hazard of this system lies in the failure to acknowledge indicators of protected access. The Veress needle is spring-loaded, and the needle "clicks" because it passes by way of the layers of the abdominal wall. At the umbilicus, two clicks ought to be felt as the needle passes through the linea alba after which peritoneum. A drop of water handed through the needle ought to fall by gravity alone into the stomach if the needle is in the right location, otherwise known as the constructive hanging water drop test. Alternately, a direct visualized entry approach with use of optical trocars may be utilized. This is especially essential if attempting to carry out a low colorectal or coloanal anastomosis. Posterior dissection below the Waldeyer fascia results in damage to the presacral veins. Although the presacral veins are a lowpressure system, they carry a significant blood volume, and enormous blood loss happens quickly. Instinctive use of cautery is regularly unsuccessful as a outcome of the veins are prone to retraction into the sacral foramina. Suture ligation or bipolar forceps can show useful but should still be insufficient, and use of further energy devices such because the argon beam coagulator and TissueLink (Medtronic, Minneapolis, Minnesota) has variable outcomes. If hemostasis has been unsuccessful with use of the previous methods, a sq. patch of rectus muscle could be harvested from the abdominal wall and sealed to the location of bleeding. With the cautery device on the highest settings and through the use of an arc welding method, the surgeon holds the cautery system barely away from the tissue and initiates welding of the muscle patch to the underlying tissue. If hemorrhage continues, pack the pelvis tightly, guarantee management, abort the procedure, close the abdomen, and have the patient taken to the intensive care unit for continued Chapter 18 Management of Bowel Surgery Complications 249 pneumoperitoneum. Although the classic two clicks of the Veress needle and hanging drop take a look at may be helpful in figuring out appropriate placement, applicable pressure from pneumoperitoneum has been proven to be essentially the most sensitive predictor of right intraperitoneal placement. If this occurs, bowel damage have to be ruled out when correct access to the abdomen has been established. If no distention is noticed with a appreciable quantity of fuel, this could be a sign that the intestinal lumen may have been accessed somewhat than the peritoneum. Trocar insertion is a controlled, penetrating stomach damage and can be treated equally to a traumatic penetrating stab wound to the abdomen. There are three consequences of trocar placement: placement into the subcutaneous tissue, entry into the peritoneum without organ damage, and entry into the peritoneum with subsequent visceral or vascular injury. Leaving the trocar in place when an harm is suspected might help make clear the trajectory of the harm and which organs may have been damaged.
Cheap alavert 10 mg free shipping
Monitor and as possible restrict the inflow of ventricular irrigation fluid to keep away from inflicting hypothermia allergy throat treatment alavert 10 mg buy cheap line. Premature infants have a circulating blood volume of about 100�110 ml/kg allergy kiosk animal kingdom alavert 10 mg mastercard, which is just barely larger than that of full-term infants. Attention to particulars and care taken preoperatively might keep away from shunt issues and malfunctions in the future. For infants with reservoirs, the identical volume may be aspirated though the reservoir with sterile approach. Overshunting also can happen in some instances, particularly in infants with extreme macrocephaly and thinned cortical mantle. In infants with severe macrocephaly, the bones of the cranium may very well erode via the skin, and in distinctive instances, cranial discount surgical procedure may be considered. Shunt valves and tubing can erode by way of the skinny, fragile skin of premature infants, so low-profile shunt methods must be chosen. Once all incisions are well healed, the shunt may be adjusted to the next setting. Often, a liquid bandage or skin glue over incisions, rather than adhesive bandages, decreases local skin injury. Careful peri-operative assessment and long-term follow-up will best avoid and reply to shunt infection and malfunction. These pointers, along with standardized protocols published by the Hydrocephalus Clinical Research Network, present best follow steering for traditional clinical scenarios. A standardized protocol to cut back cerebrospinal fluid shunt an infection: the Hydrocephalus Clinical Research Network Quality Improvement Initiative. He was born at full time period with a normal supply, after routine pre-natal care and an unremarkable being pregnant. In the previous 6 months, however, he has developed a progressively irregular gait, bent ahead. Assessment and Planning the pediatric neurosurgeon suspects a prognosis of tethered spinal wire. Toe walking in kids may result from cerebral palsy, tethered wire, or main musculoskeletal disorders, corresponding to limb length discrepancy or muscular dystrophy. Together, the constellation of findings in the present affected person, nonetheless, is highly suggestive of tethered wire syndrome. Each medical characteristic of tethered wire syndrome may be attributable to numerous other issues, however together these options are highly suggestive of the presence of spinal cord tethering: voiding dysfunction, back and leg ache, musculoskeletal and/or sensorimotor abnormalities of the distal legs and feet, and toe strolling. T1 weighted images present the neural components, dura, and different supporting structures in glorious element, and highlight fats in the filum terminale, which is common. T2 pictures are very sensitive for figuring out the precise position of the distal conus tip and in detecting spinal twine syringes. A substantial minority of sufferers with filum tethering also harbors a spinal syrinx, generally in the extra distal thoracolumbar spinal wire. Bony spina bifida occulta is extremely widespread within the basic population, particularly in children and even more so in infants. Although the conus medullaris ends barely lower than anticipated, this stage would in any other case be considerednormal. Because his signs are progressive and bodily therapy is mostly unhelpful on this condition, surgery is recommended. However, tethered cord launch ought to avoid disruption of the posterior spinal elements at this degree, and is due to this fact planned through an L3 laminoplasty, without physiological monitoring. What choices exist for the level and methodology of surgical strategy to the thecal sac for transection of the filum terminale Is physiological monitoring necessary for surgical transection of the filum terminale Patients are positioned susceptible, generally for younger kids on a standard desk with gel rolls at the chest and hips. A slight amount of mattress flexion on the stage of the hips and lumbar backbone may be added to encourage opening of the dorsal interspinous components. There are 2 options for exposing the thecal sac: interlaminar window versus single degree laminoplasty. In either case, a comparatively medial publicity totally sparing the aspect joints is appropriate. Operative photomicrograph exhibiting the laminoplasty defect, durotomy, and thickened-fatty filum terminal. Alternatively, laminoplasty may be carried out utilizing a small craniotome, or"footplate,"drill or with small Kerrison punches. Leaving the interspinous ligament on the cranial end of the publicity intact permits rotation of the lamina out of the best way and simplifies reconstruction on the finish of the procedure. A linear dural opening of only a few millimeters is adequate to identify the filum terminale, which is slightly grayer than cauda equina nerve roots and has very characteristic tortuous pial arteries. Care should be taken to separate the filum from any adherent rootlets and to cauterize its pial vasculature earlier than transecting it, as a end result of the cut finish will typically retract out of view. The intra-thecal area ought to be gently flushed with irrigation fluid prior to linear main closure utilizing a resilient permanent suture. A thin continuous layer of dural sealant is commonly used to complement the dural closure. Depending on the age of the affected person, the laminoplasty bone may be changed with suture or with a small laminar plating system. Tethered twine syndrome refers to a variable constellation of symptoms that may include neurological, musculoskeletal, gait, voiding, and ache elements. Distal thoracolumbar syringes present further oblique imaging proof of a tethered spinal cord (but in isolation may be clinically insignificant). Patients present process spinal wire detethering usually have clearly documented tethered twine syndrome as properly as imaging proof of an anatomically tethered spinal cord. In instances of diagnostic uncertainty, particularly with isolated medically refractory voiding dysfunction, urodynamic testing by an skilled pediatric urologist can determine a neurogenic sample of bladder dysfunction suggestive 36 Spinal Cord Tethering of tethered wire: detrusor-sphincter dyssynergia, reduced bladder compliance and volume, bladder hyperreflexia, and/or lowered sensation. Opening the lumbar theca within the presence of a major Chiari I malformation can cause symptomatic worsening of the Chiari and, not often, scientific decompensation. Many pediatric neurosurgeons select to decompress a Chiari I malformation when present previous to spinal cord detethering. This can be accomplished either beneath the same anesthetic or as a separate surgical encounter. However, if a conus medullaris-proximal filum cyst accompanies filum tethering, filum transection could be carried out at the caudal finish of the cyst, accompanied by cyst fenestration. The patient should be definitively confirmed to have returned to their pre-operative practical and gait standing.