Floxin
Floxin dosages: 400 mg, 200 mg
Floxin packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
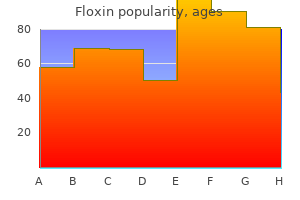
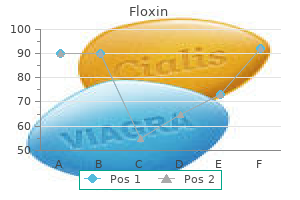
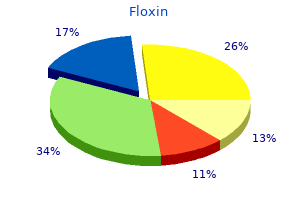
Purchase 200 mg floxin with visa
The anterior and posterior transcortical and transcallosal approaches are suitable for access not only to the lateral ventricles but additionally to the third ventricle virus 43215 generic floxin 400 mg fast delivery. The following is an outline of these approaches as used for accessing the lateral cavity antibiotics used for urinary tract infections 200 mg floxin buy with mastercard. The particular elements of third ventricular publicity with these approaches are discussed in Chapter 139. Either the cerebral hemisphere or the corpus callosum have to be traversed to reach the ventricular cavity. To reduce parenchymal traumatization by surgical manipulation, natural pathways such because the cerebral sulci, fissures, and cisterns must be used. It was Yasargil and Abdulrauf who introduced this philosophic shift from transcerebral to transcisternal planning of surgical corridors. There are two generally accepted avenues to the lateral ventricle: the transcortical and interhemispheric pathways. The choice to strategy transcortically or via an interhemispheric route is dependent upon the location and dimension of the tumor and varies on a case-by-case basis. The normal place of the patient is supine with elevation and flexion of the pinnacle. For the craniotomy, two bur holes are drilled on the contralateral facet close to the sagittal sinus. Mobilization of the draining veins is essential for gaining house, and their sacrifice ought to be prevented. This strategy is most well-liked over the use of inflexible retractors in order to protect neural structures from pressure and tearing harm. Entrance to and advance inside the interhemispheric fissure are achieved by blunt dissection with tailed cotton strips and balls. When the corpus callosum is reached, an entrance of 10 to 15 mm is generally sufficient for elimination of most lesions located in the frontal and middle components of the lateral ventricles. The smoothest method of opening is to dissect alongside the airplane of the fibers with fine-tipped bipolar forceps and small tailed cotton strips. For higher orientation within the presence of enormous tumor masses with severely distorted ventricles, the surgeon will discover the thalamostriate vein situated on the proper aspect of the plexus in the proper lateral ventricle and on the left side of the plexus in the left lateral ventricle. The additional course of the plexus and vein leads to the interior cerebral vein, which serves as a guide for localization of the fornix and thalamus and thus acts as an essential landmark. Caution needs to be taken relating to the genu of the internal capsule, which reaches the surface of the ventricle lateral to the foramen of Monro where the thalamostriate vein turns medially toward the interior cerebral vein. Instead of coming into towards the lateral ventricle by opening the center frontal gyrus as described earlier, the superior frontal sulcus is chosen for creation of the hall. The advantages and downsides are the same as described for the transcortical method. The craniotomy is positioned superior and inferior to the lambdoid suture, including the midline (as within the anterior interhemispheric approach), and may be various according to the position of the superficial bridging veins. The posterior interhemispheric fissure is then opened broadly to minimize retraction, and the precuneus and isthmus of the cingulate gyrus are opened to offer access to the ventricle. Although this method leads to direct access to the trigone, one should be aware that it poses a risk for attainable neurological issues, corresponding to visual field defects, apraxia, and acalculia. The Transsylvian Approach to the Temporal Horn the proximal transsylvian strategy was developed by Yasargil in 1967 for the therapy of vascular and neoplastic lesions in the mesial temporal space. Through a pial incision lateral to the M1 section of the center cerebral artery between the origin of the anterior temporal and temporopolar arteries, one can acquire entry to the temporal horn. In particular, limbic tumors of the amygdala, hippocampus, and parahippocampal area extending into the temporal horn could be eliminated with this approach without injuring the adjacent neocortex of the superior, middle, and inferior temporal gyrus and lateral temporo-occipital gyrus. The Anterior Transcortical Approach this route provides excellent access to the frontal horns and our bodies of the lateral cavities, and even the anterior part of the third ventricle can be exposed. This strategy is most suitable for sufferers with giant ventricles and for pathologies inside the lateral frontal horn of the nondominant cerebral hemisphere. With the affected person within the supine place and the top turned between 10 and 15 degrees to the alternative facet, the pores and skin incision and craniotomy are placed over the main a half of the center frontal gyrus. The Occipitotemporal Sulcus Approach the occipitotemporal sulcus strategy can be used to entry lesions within the posterior a part of the temporal horn. A, the affected person was placed in the supine place, and a coronal pores and skin incision has been marked behind the hairline. B, A small right-sided parasagittal craniotomy was carried out that prolonged past the midline to fully expose the superior sagittal sinus. C, Tumor exposure was obtained by way of the interhemispheric transcallosal strategy; both pericallosal arteries are stored medial by the suction tube, and a self-retaining mind retractor is inserted into the divided corpus callosum. The skin incision is bicoronal, often at the degree of or slightly behind the coronal suture. The craniotomy is usually carried out on the right side however extends slightly to the contralateral facet to fully expose the superior sagittal sinus. Small bur holes are placed obliquely within the skull at the margin of the craniotomy so that the dural flap (with its pedicle towards the sinus) may be sutured to the bone. This allows a straight-line view into the interhemispheric fissure immediately at the stage of the falx cerebri. We favor broad dissection of the interhemispheric fissure in the anteroposterior direction. In many instances, this permits working in the depth of the lateral ventricle without the utilization of self-retaining retractors. Care is taken to penetrate the corpus callosum extra laterally to avoid entrance into the ventricle on the mistaken aspect of the septum pellucidum, which can be displaced by a big tumor. This complication may be prevented by subsequent fast tumor debulking with the aid of the ultrasonic aspirator, particularly if the tumor has a high tendency to bleed in the course of the initial stage of the resection. Clinical signs arise from obstructive hydrocephalus, which leads to intracranial hypertension. In addition, cognitive adjustments are seen incessantly, especially reminiscence and attention deficits. There have been no postoperative neurological deficits; nonetheless, the patient needed placement of a ventriculoperitoneal shunt because of hydrocephalus. Histologically, this tumor reveals isomorphic nuclei in clustered patterns, a fibrillary matrix, and small cysts. Because of the benign pure history of these tumors, they remain clinically silent in many instances and are sometimes detected only throughout autopsy research. If clinical signs are absent, routine follow-up with imaging research is beneficial. If dynamic progress during follow-up or the development of medical symptoms occurs, microsurgical elimination of the mass is the treatment of alternative. In patients with existing neurological deficits caused by the remnant mass, operative resection (or finally radiotherapy) ought to be mentioned. The presence of necrosis, cysts, and calcifications in these tumors typically causes a heterogeneous look. Initially, an external ventricular drain was placed to deal with the occlusive hydrocephalus.
Trusted 400 mg floxin
There are two different widely used methods of pathologic staging of melanoma: one developed by Breslow, which makes use of invasion thickness cutoff points of 0 antibiotic with steroid discount 200 mg floxin overnight delivery. However, revisions to this technique in 2002 included the incorporation of histologic ulceration and the variety of lymph nodes involved (instead of size) to better stratify metastatic risk and patient prognosis antibiotic names cheap floxin 200 mg fast delivery. Currently, surgical margins of 5 mm are recommended for melanoma in situ, and margins of 1 cm are really helpful for melanomas as much as 1 mm in depth (low-risk primaries). Randomized prospective research show that 2-cm margins are applicable for tumors of intermediate thickness (1 to 4 mm Breslow depth), though 1-cm margins have proved efficient for tumors 1 to 2 mm in thickness. Its position is much less clear for sufferers with melanomas 1 to four mm thick, although three randomized, prospective trials failed to show elevated survival in patients with melanoma of the extremities. For later stage sufferers, larger rates of treatment failure exist, thus making adjuvant treatment incessantly needed. All are related to, at best, modest improvements in survival, though full responses have been reported in some patients. With stage Ia disease (1-mm lesions with no ulceration), the 10-year survival rate is 87. For instance, mutations in oncogenes and lack of heterozygosity of tumor suppressor genes have been a major focus of focused molecular therapies. Antiangiogenic therapies optimize the reality that neoangiogenesis is important for neoplastic proliferation. Complete surgical resection is the aim but may be difficult to realize with out affecting function. In such circumstances, radiation remedy and chemotherapy are sometimes added, either earlier than or after surgery. Adjuvant remedy is usually given in the context of a medical trial for eligible patients. In addition to the 2 extremes, numerous vascular lesions fall somewhere along the continuum from benign to neoplastic. The manifestations and treatment of some of the extra frequently occurring vascular scalp lesions are discussed here. All the tumors listed here according to the soft tissue cell of origin are comparatively uncommon. Capillary hemangiomas consist of unencapsulated collections of intently packed capillaries separated by small amounts of tissue. The lesions are typically current at birth; some have a tendency to increase in size within the first year of life and then spontaneously regress and disappear by puberty (strawberry nevus). Cavernous hemangiomas are giant, blood-filled sinuses (cavernous spaces) under the skin that seem as pink to blue spongy lesions and commonly happen on the face and scalp. In most situations these lesions are clinically benign, and as with capillary hemangiomas, they may regress over time. Both schwannomas and neurofibromas appear as raised nodules on the skin, sometimes with an overlying change in skin pigment (caf� au lait spots), and may be painful. Schwannomas are characterized by a scarcity of nerve fibers inside the tumor (fibers are displaced to one side by the mass) and have areas of high and low cellularity referred to as Antoni A and B tissue, as nicely as palisaded nuclei referred to as Verocay bodies. Neurofibromas have nerve fibers all through the lesion and are characterised by socalled spindle cells with elongated nuclei. Most neurofibromas are seen in patients with neurofibromatosis sort 1, a genetic disorder related to an abnormality on chromosome 17, although sufferers with neurofibromatosis type 2 (associated with chromosome 22) even have these tumors. In some instances the lesions could be fairly giant and type multilobar, pedunculated plenty termed plexiform neurofibromas. In rare instances these usually benign lesions progress to malignancy, corresponding to sarcoma. Removal of a neurofibroma normally requires transection of the nerve because of its intimate relationship to the body of the tumor. ArteriovenousMalformations Scalp arteriovenous malformations are high-flow vascular lesions consisting of one or more arteries that feed instantly into draining veins without intervening capillaries. In common, these lesions are sporadic, although familial syndromes that include arteriovenous malformations of the skin, lungs, brain, and different organs have been identified, similar to hereditary hemorrhagic telangiectasia and Osler-Weber-Rendu illness. Treatment of these lesions on the scalp is much like that for intracranial lesions and varies based on the dimensions, location, signs, and particular vasculature included in the malformation. Special care must be taken to establish any involvement of intracranial vessels, as well as any erosion of underlying bone. Management of scalp arteriovenous malformations might embrace embolization, surgery, or a mix of the 2. Percutaneous arterial embolization is often a helpful adjunct to surgery because it reduces blood loss and facilitates surgical approaches to otherwise unresectable lesions. Angiosarcoma Scalp angiosarcomas are rare malignant tumors of blood vessels characterised by anaplastic spindle cells and malformed vascular channels (if any are identified at all) lined with poorly differentiated endothelial cells. Potential danger factors embody increasing age, radiotherapy, publicity to arsenic compounds, and solar publicity. They tend to be multicentric, strong, closely vascular, and domestically aggressive, with microscopic tissue invasion. Because preliminary tumor measurement is a crucial prognostic issue, early detection and therapy are essential. Hair follicle tumors include several benign lesions corresponding to trichogenic tumors and pilomatricoma, as properly as a extra malignant model termed trichilemmal carcinoma. Tumors of the glandular system embrace nevus sebaceus of Jadassohn (of curiosity primarily for its potential for malignant conversion), sebaceous hyperplasia and carcinoma, apocrine and eccrine hidrocystomas, apocrine syringocystadenoma papilliferum, cylindroma, spiradenoma, and adenocarcinoma. All these lesions are extraordinarily uncommon and are typically detected clinically as raised, asymptomatic nodules on the scalp. It should be saved in mind that a few of these lesions are aggressive and may (rarely) metastasize. Lesions are regularly seen on the pores and skin, including the face and scalp, and seem as multifocal purple to violet patches. Treatment ought to be individualized however may embody surgical excision, radiotherapy, chemotherapy, and discontinuation of immunosuppressive therapy. There are reports of metastatic scalp lesions for nearly all the more commonly occurring major cancers, together with breast, lung, and melanoma. Treatment of these lesions varies by main location, medical situation of the patient, and variety of lesions. If the patient is medically steady, resection is suggested as a result of it could enhance survival in some situations. Intracranial primary tumors (usually meningiomas) could spread to the scalp after eroding bone. In common, the relatively rare schwannomas are extra likely to be solitary and encapsulated, and neurofibromas are more likely to be multiple and unencapsulated. Nonsteroidal anti-inflammatory medicine and the chance of actinic keratoses and squamous cell cancers of the skin. Incidence of cutaneous melanoma amongst non-Hispanic whites, Hispanics, Asians, and blacks: an evaluation of California Cancer Registry knowledge, 1988-93. Aesthetic reconstruction of enormous scalp defects by sequential tissue growth without interval.
Floxin 200 mg with visa
Incision of the tela choroidea lateral to the fornix and dissection of the interior cerebral veins and the medial posterior choroidal artery provide access to the third ventricle antibiotic 5 day treatment floxin 200 mg lowest price. The Anterior Interhemispheric Transcallosal Paraforniceal Approach After sufficient publicity and reflection of the dura mater, the interhemispheric house on the best facet is dissected right down to the anterior portion of the corpus callosum commonly used antibiotics for sinus infection floxin 200 mg cheap on-line. The corpus callosum is incised medial to the pericallosal artery, and the best lateral ventricle is opened. In lesions that have already enlarged the foramen of Monro, no further action may be essential. This approach is appropriate for getting entry to the anterior two thirds of the third ventricle from the roof to the bottom. Dissection begins lateral to the proper fornix on the posterior margin of the foramen of Monro, and the tela choroidea is steadily incised. Dissection is carried out between the two inside cerebral veins while being cautious to avoid the medial posterior choroidal artery. After incising the inferior membrane of the tela choroidea and mobilizing the choroid plexus of the third ventricle, the proper fornix is gently mobilized toward the opposite side, and the right thalamus (including the thalamostriate vein) may be visualized posteriorly as a lot as the posterior commissure and superiorly to the splenium of the corpus callosum (see Video 138-4). D, Both lesions had been eliminated via a proper frontal transsulcal, transcortical access route with the affected person in the supine place; a coronal skin incision behind the hairline was used. Initially, endoscopic ventriculocisternostomy was carried out at one other institution. D, Subsequently, the tumor was eliminated through the interhemispheric transcallosal paraforniceal method with the patient placed within the supine place. Gross-total elimination of the tumor was achieved through the mixed supracerebellar infratentorial and right occipital transtentorial access route. Preoperatively, the patient suffered from diffuse headache, vertigo, urinary disturbance, and hiccups. All signs gradually improved after surgery, and there was no further morbidity. The Occipital Transtentorial Approach to the Pineal Region this approach is best suited for sufferers with a good infratentorial house or large tumors of the pineal region with significant caudal extension that requires an adequate superior to inferior viewing trajectory. The distinction between our technique and the usual strategy (see earlier) lies in the truth that we prefer to combine the supratentorial craniotomy with an infratentorial craniotomy extending bilaterally to the midline. Surgery is begun by opening the cerebellar dura under the transverse sinus on both sides. This permits inspection of the supracerebellar bridging veins earlier than exposing the supratentorial area (see Video 138-5). Incision of the tentorium just lateral to the straight sinus could be carried out extra safely with precise data of the infratentorial venous sample. Moreover, dissection of the agency arachnoid surrounding the tectal plate and the vein of Galen can simply be carried out before incising the tentorium from the infratentorial path initially of the procedure. This facilitates orientation and subsequent dissection from the supratentorial path. Great attention is paid to the superficial cerebellar veins, which are at all times preserved. Usually, these lesions are positioned more or less within the midline; nevertheless, they can be accessed unilaterally by way of the infratentorial supracerebellar house. In all circumstances, the arachnoid that surrounds the tectal plate and the veins that drain into the vein of Galen are dissected meticulously to obviously establish all anatomic constructions within the region. E, Intraoperative photograph of the supracerebellar infratentorial surgical method that was used. The cerebellar culmen has been gently mobilized inferiorly, and the tumor is visible within the neighborhood of the vein of Galen. F, Macroscopic side and histologic specimen of the lesion confirmed as a fibrillary astrocytoma. This pathology was first described by Wallmann in 1858 as an post-mortem discovering, and Walter Dandy was the first to efficiently take away this kind of tumor in 1921. The tumor can stay clinically silent for a very lengthy time and is subsequently usually detected only at post-mortem. Colloid cysts can attain a big volume that probably occludes the foramen of Monro and results in acute, obstructive hydrocephalus. The episodic appearance of symptoms with irregular symptomfree intervals makes the prognosis somewhat challenging based purely on medical examination. Other symptoms arising from elevated intracranial pressure embody nausea, vomiting, dizziness, and fatigue. A sudden enhance in intracranial stress from rapid-onset hydrocephalus can result in sudden death. Differential prognosis includes neurocysticercosis, intracranial aneurysm of the posterior circulation, and vertebrobasilar dolichoectasia. The radiologic appearance is dependent upon the amount of gelatinous material inside the tumor. The only definite therapy of this pathology is resection of the cyst by microsurgical or endoscopic techniques. Neuronavigation serves as an essential device to additional optimize the surgical trajectory and improves the safety and efficiency of operative interventions. In any case, rupture of the cyst should be prevented because this can result in ventriculitis and meningitis. Clinical proof of third ventricular ependymomas results primarily from obstructive hydrocephalus with a consequent improve in intracranial pressure and cognitive deficits. Removal continues to be within the domain of microsurgery, however there are reports of profitable elimination purely by endoscopic approach. Initially, an exterior ventricular drain was placed to release the raised intraventricular pressure. They have two incidence peaks, between 5 and 10 years and between 45 and 60 years of age. With increasing volume, they tend to displace surrounding neuronal and vascular constructions and might doubtlessly invade the third ventricle. Its microscopic features embrace squamous epithelium, lobules, palisades, and cysts full of particles. The lesion may be accessed either by the anterior interhemispheric subfrontal strategy. In latest years, successful remedy by endoscopic method has additionally been reported; cystic intrasellar tumors are particularly appropriate for this therapy. Moreover, tumor resection and additional resolution of tumor-related hydrocephalus may be achieved on the similar time. They originate from the thalamic or hypothalamic regions or from areas of the midbrain, they usually expand into the third ventricle. Depending on their nature, they turn into clinically evident by displacing or infiltrating the surrounding anatomy. By compromising these neuronal buildings, symptoms similar to endocrine imbalance, intracranial hypertension, and visible and cognitive impairment occur.
Order floxin 400 mg visa
If wanted, a dural replacement graft is inserted and microscopically sutured to achieve watertight closure antimicrobial resistance fda floxin 400 mg buy low cost. With the high-speed drill, osteotomies are made in the ground of the anterior cranial fossa antibiotics used to treat bronchitis buy floxin 200 mg lowest price. If the tumor entails the whole ethmoidal sinus complex, these osteotomies should be positioned by way of the medial a half of the orbital roof to enter the orbits bilaterally, lateral to the lamina papyracea. This suture overlies the posterior ethmoidal air cells in most people, though it could overlie the anterior half of a giant sphenoidal sinus. As talked about, the posterior ethmoidal foramen is within the posterolateral side of this osteotomy. The exit of the optic nerve from the optic canal may be discovered roughly 5 to 7 mm posteromedial to this artery. From above, the periorbital membrane is dissected from the lamina papyracea bilaterally, and a small curved osteotome is positioned medial to the orbital tissues. An osteotomy is made at the inferior facet of the lamina papyracea simply the place the bone turns to form the ground of the orbit. An osteotomy is then fashioned throughout the lamina papyracea posteriorly, with half of the osteotome being intraorbital and half within the posterior ethmoidal sinus. The anterior osteotomy is carried out across the base of the frontal sinuses and enters the nasal cavity. The anterior part of the nasal septum may be uncovered right here and is divided with heavy scissors, which permits removal of the entire specimen transcranially. Residual air cells are removed, and any involved or questionable periorbital tissue is resected. Small periorbital defects are nicely tolerated, but massive defects must be repaired with temporalis fascia. The pericranial flap is then reduce to the appropriate size and sutured to drill holes positioned within the planum sphenoidale and medial orbital roofs. Fibrin glue could additionally be used to strengthen the dural restore and the perimeters of the pericranial graft. It is vital to determine that no compression of the pericranial graft is being caused by the bone flap. Invasion of the orbital wall happens in 60% to 80% of patients with ethmoid or maxillary sinus malignancies. McCary and colleagues reported that only four of 36 patients (11%) whose eyes have been spared had recurrence Sphenoidal Internal sinus carotid a. Temporal dura Periorbital membrane Transmaxillary Maxillary Neurectomy Achieving microscopically tumor-free margins throughout resection of cranium base malignancies has consistently been identified as a optimistic prognostic factor for affected person survival. Traditionally, when malignancies have prolonged perineurally into the intracranial portion of the maxillary nerve and anterolateral cavernous sinus, a temporal craniotomy was used to entry this area for resection. The amount of bone resected is determined by the extent of the tumor and should contain a medial, inferior, or complete maxillectomy. The infraorbital nerve is identified and adopted to the pterygomaxillary fissure. The nerve is dissected free of adipose tissue and adopted to the foramen rotundum, located on the top of the pterygoid plate. The foramen is widened with a high-speed drill to expose the dura of the temporal fossa ground laterally and the cavernous sinus medially. The medial temporal dura is dissected laterally from the maxillary nerve in its course through the lateral wall of the cavernous sinus. In a clinical collection with a predominance of advanced squamous cell carcinoma, there was solely a 30% survival price (10 of 34 patients) in those that had preservation of the orbital contents versus a 50% survival rate (28 of 55 patients) in those present process resection. Few eye issues occurred within the 10 sufferers in whom the orbital ground was preserved, especially if the eye was not included in the radiation area. These authors concluded that when the orbital ground is resected and the radiation subject will embrace the eye, exenteration must be carried out. Adverse orbital outcomes have been shown to be strongly related to resection of the orbital flooring and resection of two thirds or more of two or more orbital walls. The temporalis fascia on the aspect of the orbitectomy is incised from the extent of the superior temporal line to the basis of the zygoma. Depending on whether or not the tumor is anterior or posterior in the orbit, the orbital rims may be left in place and taken as part of the specimen or eliminated and changed on the finish of the operation. The temporalis muscle is fastidiously dissected from the temporal fossa and mirrored posteriorly whereas ensuring that its blood supply is preserved. The higher wing of the sphenoid is eliminated with a high-speed drill to expose the superior and inferior orbital fissures. The lesser wing of the sphenoid, which makes up the posterior a part of the orbital roof, is left in place as a information for the orbital incisions. Beginning laterally just at the degree of reflection of the temporal dura to the superior orbital fissure, the tissues of the superior and inferior orbital fissures are incised flush with the bone of the orbit with chopping cautery. As this cut progresses medially, care is taken to establish the ophthalmic artery, which is coagulated and divided; the incision then continues through the optic nerve. A high-speed drill is used to go through the ground and medial wall of the orbit for entrance into the maxillary sinus and posterior ethmoidal sinuses, respectively. A bifrontal or unilateral frontal craniotomy is fashioned, and the subfrontal dura is elevated as described beforehand. The osteotomies are positioned by way of the cribriform plate into the ipsilateral ethmoidal sinuses if the tumor is completely within the orbit, into the contralateral ethmoidal sinuses if extension by way of the medial orbit occurs, or probably even into the contralateral medial orbit if the whole ethmoid complicated needs to be resected. An osteotomy through the rest of the orbital roof completes the superior osteotomies. If the tumor extends posteriorly into the orbital apex, the lesser wing of the sphenoid is eliminated, including the anterior clinoid, and the optic canal is opened. The subclinoid inner carotid artery is identified, and the optic nerve and ophthalmic artery are divided throughout the optic canal. Using a high-speed drill, an osteotomy is made by way of the ground of the optic canal into the underlying sphenoidal sinus. Care is taken to stay anterior to the anterior loop of the internal carotid artery. The transfacial method is then used to perform either partial or whole maxillectomy. If solely partial maxillectomy is required, it can be carried out utterly via the circumorbital incision. If complete maxillectomy is required, a lateral rhinotomy and lip-split incision could additionally be wanted. Reconstruction can usually be carried out by utilizing the pericranial flap previously harvested and the temporalis muscle with a pores and skin graft. Most commonly, lateral exposure is required for tumors of the maxillary sinus that invade by way of the posterior wall and enter the infratemporal fossa. This maxillary sinus leiomyosarcoma with infratemporal fossa extension required a lateral approach for en bloc tumor resection. A preauricular incision is used, which may be extended across the scalp into a full bicoronal or three-quarter bicoronal incision, depending on the quantity of anterior publicity wanted. The incision may also be extended down into the neck to permit parotid and neck dissection or mobilization of the mandible.
Generic 200 mg floxin mastercard
Patients with recurrent tumors could also be helped with extra surgical procedure, radiotherapy, and chemotherapy virus 10 states order floxin 400 mg on-line. Anterior craniofacial resection for malignant ethmoid tumors-a collection of ninety one sufferers antibiotics for uti macrobid order 400 mg floxin otc. Transmaxillary exploration of the intracranial portion of the maxillary nerve in malignant perineural disease. Ophthalmological outcome after orbital entry throughout anterior and anterolateral cranium base surgical procedure. Post-operative intensity-modulated radiotherapy for malignancies of the nasal cavity and paranasal sinuses. Prognostic significance of transdural invasion of cranial base malignancies in sufferers present process craniofacial resection. Surgical results of cranium base surgical procedure for the therapy of head and neck malignancies involving cranium base: multi-institutional studies on 143 circumstances in Japan. Craniofacial resection for malignant paranasal sinus tumors: report of an International Collaborative Study. Craniofacial resection for tumors of the nasal cavity and paranasal sinuses: a 25-year experience. The treatment of superior sinonasal malignancies with pre-operative intra-arterial cisplatin and concurrent radiation. Anterior transcranial (craniofacial) resection of tumors of the paranasal sinuses: surgical technique and results. Occupational dangers for adenocarcinoma of the nasal cavity and paranasal sinuses in the German wood business. Jane Sr Esthesioneuroblastoma, first described by Berger, Luc, and Richard in 1924,1 is an unusual neoplasm that arises from olfactory epithelium excessive within the nasal vault and frequently invades the cranium base, cranial vault, and orbit. Although esthesioneuroblastoma accounts for as much as 3% of intranasal neoplasms in some collection, fewer than 400 distinctive cases have been reported on the planet literature. The recent apparent enhance in incidence is at least partially attributable to improvements in diagnostic imaging and pathologic recognition of this comparatively rare entity. Because of the restricted variety of topics handled in numerous eras of medical and surgical apply, in addition to nonuniform therapy schemes and follow-up, management recommendations relating to these tumors have been primarily based largely on anecdotal information and limited collection. Evaluation by an otolaryngologist is warranted each to assess the extent of sinus and cervical disease and to provide a diagnostic biopsy specimen. A preoperative neuroophthalmologic analysis should be performed to establish visual acuity or motility deficits and to doc baseline function in sufferers with disease close to orbital constructions or in whom in depth surgical resection is anticipated (Table 143-3). Adequate radiographic evaluation allows preoperative classification of the tumor according to the scheme proposed by Kadish and modified by others (Table 143-4). Patients in whom metastatic disease is suspected ought to bear a radical analysis for dedication of the extent of illness and number of adjuvant therapy. Light microscopy reveals a lobular structure with sheets of cells in a dense neurofibrillary background. A grading system primarily based on histology has been proposed as a prognostic device but has achieved varying success (Table 143-1). A fleshy, friable nasal mass is incessantly noted, and hyposmia is commonly detected on formal testing. Other, much less widespread initial symptoms and signs include headache, visual impairment, and rhinorrhea (Table 143-2). Metastatic disease is current in 17% to 48% of sufferers with esthesioneuroblastoma at analysis. This effort has been additional hampered by the adjustments in medical administration, surgical approach, and expertise over the previous 50 years; sufferers in early reviews have been treated in a much totally different era of medication than these lately. With the onset of interest in cranial base surgical procedure, remedy paradigms have shifted from much less aggressive surgical resection to more frequent complete resections. More lately, interest has begun to shift to less invasive, endoscopic-assisted surgical intervention with adjuvant stereotactic delivery of radiotherapy or radiosurgery. Although expertise with adjuvant therapies has been restricted, some benefit appears to be gained from the utilization of radiotherapy and chemotherapy. However, based mostly on our experience with the use of radiosurgery for focal areas of recurrent illness, major definitive radiosurgery could also be a legitimate plan for stage A and selected stage B tumors. Theoretical advantages of preoperative radiation remedy embody decreasing tumor mass and minimizing native tumor dissemination and distant metastases at the time of surgery by lowering cell viability. Preoperative tumor irradiation has proved helpful in sparing the orbital contents throughout surgery for paranasal sinus carcinoma. In a series from the Mayo Clinic, the incidence of recurrence of both high- and low-grade tumors was decreased by postoperative radiation therapy. For patients with superior or metastatic illness, adjuvant therapy might present further profit. Improved outcomes have been reported for sufferers undergoing neck dissection and radiation remedy for cervical illness. Probably because of this, similar chemotherapeutic regimens found to be efficient for these other lesions have been used for esthesioneuroblastoma, with variable results. B, Specimen from a better grade tumor showing more cellularity with less tissue architecture. Tumor extends from the ethmoidal sinuses and nasal vault via the cribriform plate and into the intracranial compartment (arrows). Typically, regimens embrace cyclophosphamide and vincristine, although doxorubicin is sometimes included. A few facilities have used high-dose chemotherapy with bone marrow rescue and intra-arterial chemotherapy with some success as well. Patients with Kadish stage A or B tumors received 45 to 50 Gy of radiation preoperatively; patients with Kadish stage C lesions underwent the same dose of radiation along with six cycles of cyclophosphamidevincristine (20 patients) or cisplatin-etoposide (3 patients) chemotherapy. Our remedy routine was related to a decrease in complete tumor volume of higher than 50% or a discount in intracranial tumor mass of greater than 90% in thirteen patients (54%). Interestingly, the only patient with progression of tumor through the interval of chemoradiation therapy obtained methotrexate as an alternative of cyclophosphamide. The sum of the experience with chemotherapy and radiation therapy for esthesioneuroblastoma means that some benefit is afforded by these therapies; nonetheless, the limited variety of subjects and variability in treatment protocols have limited the development of definitive recommendations. In sufferers not medically precluded from surgical procedure, resection seems to improve long-term outcomes. Smith and colleagues described a combined transfacial and transcranial method for resection of paranasal sinus carcinoma in 1954,27 and in 1970, the first craniofacial resection for esthesioneuroblastoma was carried out by Drs. Soon thereafter, boosted by the reports of Ketcham and associates and Clifford, the use of craniofacial resection for tumors on this area turned widespread. The limits of tumor resection were prolonged, and enhancements in consequence followed. Our experience on the University of Virginia with 50 sufferers showed disease-free survival rates of 86. However, published stories have demonstrated success with radiosurgical remedy of recurrent or residual disease. Radiosurgery could additionally be sophisticated by the issue of figuring out an correct target in the setting of postoperative modifications, together with intensive packing for cranial base reconstruction.
200 mg floxin generic with mastercard
A 63% radiographic response fee and a 38% 6-month progression-free survival rate was reported with an acceptable aspect effect profile antibiotics for acne azithromycin floxin 200 mg cheap visa. As our understanding of the molecular biology of these tumors expands, so do options for rational therapy methods treatment for viral uti buy floxin 400 mg without prescription. Epidermal progress factor receptor and glioblastoma multiforme: molecular basis for a model new strategy. Therapeutic advances in the treatment of glioblastoma: rationale and potential role of targeted agents. Changing paradigms-an update on the multidisciplinary management of malignant glioma. Transforming growth factor-beta: a molecular goal for the longer term therapy of glioblastoma. Sphingosine1-Phosphate Sphingosine 1-phosphate (S1P) is a lipid that can act as a glioma cell mitogen through activation of one of 5 G protein�linked receptors. Two farnesyltransferase inhibitors, tipifarnib (Zarnestra) and lonafarnib (Sarasar) have proven modest encouraging leads to a number of forms of cancers. A regular cell will carefully control its development past development or repair/regeneration, however a cancer cell has uncontrolled progress prompted by pathologic directions from the mutated genome. A normal genome will instruct a cell to coexist with its neighboring cells, whereas a brain cancer cell with mutations will invade and finally destroy the encompassing mind. Alterations in a mind cell genome at crucial areas, inside genes that management cell development, cell cycle, and cell dying, are the premise for the formation of brain tumors. For a small proportion of mind tumors, the first mutation is inherited from one of many parents and increases the risk for the event of a mind tumor, though the next mutations needed to complete tumor formation are acquired in the identical method as spontaneous tumors. There are external causes that significantly improve the risk for development of a most cancers, however for brain tumors the evidence for this is restricted. A high dose of ionizing radiation to the brain has the strongest evidence for rising the risk for sure mind tumors, as seen with radiation therapy involving the brain1 or will increase in meningiomas in atomic bomb survivors. Certain artificial chemical substances, corresponding to fungicides and pesticides, show an association of publicity to elevated incidence,4,5 but more analysis is required to demonstrate a direct cause-and-effect relationship. It is obvious, nevertheless, that the quantity and complexity of mutations arising during malignant tumor development, together with mind cancers, are a lot greater than initially predicted. Understanding the function and mechanisms of these pathways will produce higher insight into how tumors proliferate and thus provide researchers with better means for molecular focusing on. As mutations in important genes accumulate in a cell, a cancer develops in stepwise fashion. This is often true, besides in a couple of situations, such because the presence of unstable amplifications that give rise to heterogeneity for this change in the tumor or the acquisition of a late-occurring mutation within the latter levels of tumor cell clonal expansion. For the overwhelming majority of mutations, nevertheless, the same mutations will seem in all parts of the tumor. Linkage and affiliation research can locate the approximate region of the chromosome liable for a disease phenotype primarily based on discovering a polymorphic marker that cosegregates in households with people affected by the disease. Because the primary hit is inherited as a germline mutation, it can be transmitted to offspring. Table 102-1 lists some of the extra widespread cancer-associated mendelian disorders which have brain tumors as a half of the phenotype. Mendelian problems are genetic illnesses which have a transparent sample of inheritance within families, such as dominant or recessive inheritance. Most of the syndromes that involve brain tumors have an autosomal dominant mendelian inheritance sample. The traditional scenario for a brain tumor phenotype with mendelian inheritance is the dominant inheritance of a mutation in a tumor suppressor gene, with a mean of 50% of offspring inheriting one copy of the mutated gene from the affected parent. In the case of tumor suppressor genes, each copies need to be inactivated to provoke the process of tumor formation. Although most mendelian issues that embody within the phenotype an increased threat for brain tumors are comparatively uncommon in the general population, there are some exceptions. Neurofibromatosis is the most common of the syndromes with mind tumors as a phenotypic function. In roughly 10% or much less of these patients, a malignancy will develop from considered one of their multiple benign tumors. Therefore, a mutation in any of these genes can result in an elevated danger for mind and different cancers. Inherited patterns assist researchers locate the genes that may provoke brain tumors, and figuring out a familial danger for cancer can be good clinical apply. Identifying the gene accountable gives the patient choices for genetic counseling and family planning, in addition to provides the opportunity for early analysis and therapy of other relations carrying the disease-causing gene allele. In some cases, figuring out a cancer syndrome in a family may be lifesaving for a member of the family. Gain-of-function mutations are adjustments that both enhance the conventional gene operate or add a new function. Gain-of-function mutations are activating and change a proto-oncogene to an oncogene. Activation of an oncogene then contributes functionally to tumor progression, in live performance with different gene mutations. Occasionally, splicing-related mutations that add or delete gene exons can activate an oncogene. Mutations that produce a brand new cease codon (truncating mutation), delete all or part of the gene, disrupt the gene promoter, alter splicing, or change an amino acid or acids rendering the protein nonfunctional are all widespread methods to inactivate a tumor suppressor. This elevated mutation price then results in important mutations in oncogenes and tumor suppressors, though many new mutations will occur all through the whole genome. The resulting accelerated mutation rate then leaves the cell primed to activate oncogenes and inactivate tumor suppressors at an accelerated rate. When the number of alleles is increased considerably beyond the conventional two copies, it is named genomic or gene amplification. The presence of increased copy numbers of a gene on account of genomic amplification is a dependable indication that an oncogene is located in the amplified region. Either the traditional gene may be discovered to be amplified (and simply will increase its regular function to pathologic levels), or a mutated oncogene could be discovered within the amplified area. Mutated genes also can arise in genomically amplified areas, and the mutation would possibly happen either before or after the amplification. In the coding regions of genes, a degree mutation that alters the three-letter genetic code in such a means that the amino acid is modified is known as a nonsynonymous change. Normally, these silent adjustments are regarded as nonfunctional, however there may be hidden regulatory sequences throughout the coding region that can cause a functional change. Point mutations can also change an amino acid to a stop codon and, along with different mutations that induce early termination of protein translation, are known as truncating mutations. Point mutations and other modifications can even alter gene regulatory regions within the gene or at regulatory areas distant from the gene. Other common small mutations can alter gene splicing, alter transcript levels, or type new proteins. Insertion and deletion of a number of bases can have the identical impact as level mutations. New amino acids can be added or deleted to a protein and thereby either activate a model new operate or delete the traditional perform.
Buy floxin 400 mg lowest price
Transsphenoidal resection of the lesion is mostly the most secure technique for intrasellar tumors virus 4 free floxin 400 mg generic overnight delivery. In specific cases, radiation therapy is used as an adjunctive measure after surgical procedure to prevent recurrences; thus, it may be postponed until after delivery antibiotic home remedies order floxin 400 mg without prescription. The security of continuous bromocriptine or octreotide remedy has not been totally assessed, and women ought to be advised to discontinue such remedy after being pregnant is confirmed. Periodic assessment of visual fields every 3 months in women with microadenomas and every 6 weeks in these with macroadenomas has been really helpful. Nonetheless, only a small percentage of pregnant ladies with pituitary adenomas require additional surgical therapy earlier than delivery. Finally, the notion that breastfeeding induces the expansion of prolactin-secreting adenomas ought to lead to specific vigilance when managing women with bigger tumors in the course of the puerperium. Their figuring out signs may be the outcome of direct damaging or irritative effects on the surrounding nervous tissue or elevated intracranial stress. Although focal neurological deficits or seizures can be clear identifying indicators, symptoms ensuing from elevated intracranial pressure, such as headache, drowsiness, nausea, and vomiting, are much tougher to inform apart from the traditional discomforts of being pregnant. In these circumstances, accompanying indicators such as papilledema, subtle changes in psychological standing, cranial nerve deficits, and motor or sensory dysfunction help in diagnosis. These diagnostic tests provide precise data on the configuration of the lesion, its relative vascularity, the presence of cystic parts or concomitant obstructive hydrocephalus, and the diploma of compression of surrounding structures. These imaging research also can present data on the histologic kind and grade of the malignancy. Electroencephalography is usually helpful for the optimum administration of seizures. Treatment Two forms of agents are used to manage the symptoms associated to glial tumors: corticosteroids and anticonvulsants. Synthetic corticosteroids, corresponding to dexamethasone and methylprednisolone, are used to ameliorate perineoplastic brain edema. Corticosteroids control the progression of symptoms and assist in suspending surgical intervention. As with different brokers for which teratogenicity has not been determined, nonetheless, unless the benefits of remedy clearly outweigh the potential hazards to the mother and fetus, the use of corticosteroids is discouraged during early pregnancy. An various approach ought to be taken in pregnant women, nevertheless, due to the affiliation of anticonvulsants with teratogenicity. To date, no conclusive info is available on which of the four major antiepileptic drugs (phenytoin, carbamazepine, valproate, and phenobarbital) is probably the most teratogenic. If a single focal seizure is reported, initiation of anticonvulsant remedy ought to be deferred if possible. If the intracranial stress is a results of obstructive hydrocephalus, a shunting procedure should be performed. Recent technologic advances have launched precision stereotactic equipment that enables extraordinarily correct biopsies with a low price of morbidity. Limited diagnostic biopsies are carried out for deep-seated lesions, for tumors in direct proximity to eloquent portions of the cortex, or for significantly high-risk patients when a reliable tissue prognosis is required. In each conditions, the patient have to be monitored by frequent neurological examinations and neuroimaging research, and if wanted, medical therapy should be undertaken all through the being pregnant. Irradiation and chemotherapy are each generally used to treat sufferers with malignant gliomas. If treatment is required throughout being pregnant, nonetheless, it is very important take precautions to guard the fetus. Conventional radiation therapy is important within the therapy of glial tumors as an adjuvant measure after surgery. Stereotactic radiosurgery, which uses precisely defined converging radiation beams such as with the Gamma Knife and linear accelerator modalities. Chemotherapeutic agents must be prevented during the first trimester of being pregnant. Treatment Management of meningiomas throughout being pregnant must be tailor-made on an individual basis. If surgical resection is the only conclusive treatment of these benign tumors, nevertheless, it can be carried out throughout pregnancy. Its signs, corresponding to headache, dizziness, vomiting, blurred vision, paresthesias, and tinnitus, are sometimes just like these of a mind tumor. Frequently, patients experience progressive visual impairment, in all probability resulting from continual papilledema. The trigger is still unclear, but several factors have been advocated, together with elevated cerebral blood volume, endocrine dysfunction, vascular obstruction of the draining sinuses, and electrolyte imbalance. Patients with pseudotumor cerebri ought to have periodic full ophthalmic evaluations. Medical treatment with small doses of corticosteroids and acetazolamide or different diuretics frequently helps control signs. In these cases, surgical nerve sheath decompression has been proposed as a substitute for shunt placement. These benign tumors could progress rapidly during being pregnant, and signs could disappear after delivery. Acoustic neuromas,132 ependymomas,127 medulloblastomas,133 and choroid plexus papillomas134 have reportedly been found in pregnant women. The incidence of primary mind lymphoma has elevated with the rise within the prevalence of acquired immunodeficiency syndrome. Their therapy is mostly palliative and varies based on the nature of the primary tumor and the extent of the systemic and central nervous system dissemination. Evidence means that surgical resection followed by radiation remedy produces the best probability of survival in patients with surgically accessible, solitary brain metastases. Although melanoma, breast cancer, and lung cancer are statistically the tumors that metastasize to the mind most incessantly, choriocarcinoma also has a propensity to happen during being pregnant, and mind metastases are probably the most frequent neural complication. The physiologic modifications that occur during pregnancy have been proven to influence the severity and period of symptoms related to tumors and, specifically, with pituitary adenomas, glial tumors, meningiomas, and vascular tumors. If surgery is important, nevertheless, enhancements in surgical and anesthetic strategies permit us to function with minimal detriment to the patient and the fetus. Hence, the scientific conditions of most pregnant sufferers with major or metastatic brain tumors may be controlled without untimely termination of their pregnancies. Establishing the factors for anesthesia and different precautions for surgical procedure during pregnancy. Pituitary gland development throughout normal being pregnant: an in vivo examine using magnetic resonance imaging. Reproductive factors and the risk of brain tumors: a population-based examine in Sweden. Antiepileptic drugs and teratogenesis in two consecutive cohorts: modifications in prescription coverage paralleled by changes in sample of malformations. Chang the primary line of remedy for primary mind tumors is surgical procedure and radiation, yet these modalities alone are hardly ever curative for malignant tumors. Cell cycle kinetic studies have proven that the cells that migrate into regular mind are the most viable and have the highest capacity for proliferation. It was solely lately that chemotherapy became a standardized part of the treatment for newly recognized major tumors.