Lady era
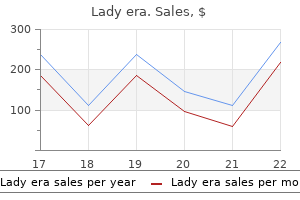
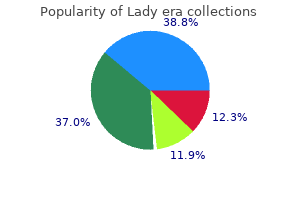
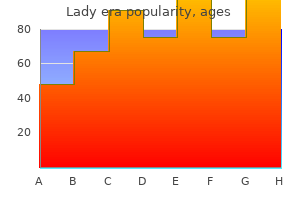
Lady era dosages: 100 mg
Lady era packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Generic 100 mg lady era visa
The vary of transfer ments supplied by these joints and the muscles acting throughout them is big menstruation 2 lady era 100 mg purchase free shipping. Arthrodesis of the thoracoscapular joint is effective in scap ulohumeral dystrophy; it restores full elevation of the limb however protrac tion and retraction is misplaced general women's health issues generic lady era 100 mg with visa. A appropriately performed glenohumeral arthrodesis retains highly effective adduction, protraction and medial rota tion, however lateral rotation and most of elevation are lost. The elbow includes a hinge between the humerus and ulna, and two pivot joints: one between the humerus and radius, the opposite between the proximal radius and ulna. This permits a spread of about 150� of extension and flexion, and 180� of pronosupination along side the distal radioulnar joint. The wrist complex allows a spread of flexion and exten sion of about 140�, supplemented by some 70� of adduction and abduction. The condylar metacarpophalangeal joint enables 120� of flexion and extension, about 40� of abduction and adduction, and a few rotation. The penalties of scarring from burn or other harm, or badly placed incisions, are extreme, and nowhere more so than after a deep burn of the axilla. The superficial fascia (see Chs 2 and 29) is generally thicker on the dorsal side of the neck, shoulder, arm and forearm. This fascia is a vital gliding plane between the skin and the underlying deep fascia. Nerves and vessels are susceptible to entrapment and even rupture the place they perforate the deep fascia to ramify into the superficial fascia and skin. The deep fascia, intermuscular septa and the interosseous membrane between the radius and ulna outline discrete compartments that allow gliding of segregated buildings in opposition to each other. The medial and lateral intermuscular septa of the arm and the interosseous membrane also provide extensive areas for the attachment of muscular tissues. The varied fascial compartments are related to the unfold of an infection and tumour, and are especially important in ischaemia. It tasks under the clav icle as the axillary sheath, enveloping the divisions and cords of the brachial plexus with the axillary artery, and continues into the arm because the brachial sheath, surrounding the brachial artery with its venae comitantes, the median nerve and the proximal a part of radial and ulnar nerves. The great muscular tissues of the shoulder and axilla � deltoid, pectoralis main and latissimus dorsi � are coated by deep fascia that winds round their deep surfaces to mix with the deep fascia of the arm. This latter is drawn upwards by suspensory condensations of fascia to kind the coneshaped axillary space. This association is clear to the reader who traces the anterior surface of pectoralis main with a finger, then follows it round and deep, before thrusting the finger upwards as far a minimal of because the lateral a part of the second rib. The deep fascia of the arm and forearm types a sort of sleeve, hooked up to the medial and lateral intermuscular septa within the arm, to the periosteum of the medial and lateral epicondyles and olecranon at the elbow, and to the periosteum of the ulna and radius (Chs 48�49). There are necessary condensations, such because the bicipital aponeurosis on the elbow, and the flexor and extensor retinacula at the wrist, which are, in turn, subdivided by septa. Discrete compartments with the forearm separate the superficial muscle tissue from the deep. The deep flexor compartment incorporates the anterior interosseous nerve and vessels, flexor pollicis longus, flexor digitorum profundus and pro nator quadratus. The superficial compartment incorporates the radial artery, pronator teres, flexor carpi radialis, palmaris longus and flexor digit orum superficialis. The vary of excursion of the main nerves of the upper limb throughout mounted factors similar to the first rib, the distal humerus and the distal radius is a few 10�15 mm and is enabled by gliding between the adventitia and the epineurium. More movement happens within the plane between the epineurium and perineurium, and likewise inside the perineurium itself (Commentary 9. Cutaneousinnervation Bundles of nerves enter the skin deep in the dermis and course in the direction of the pores and skin surface, giving off axons, practically all unmyelinated, that internal vate the associated end organs. The few myelinated axons terminate at hair follicles, Meissner corpuscles and Merkel complexes (Ch. The postaxial pores and skin of the posterior aspect of the neck, shoulder, arm and forearm is thicker and hairy, whereas the glabrous preaxial skin on the anterior floor of the arm and forearm is thinner and more mobile. The state of affairs is reversed within the hand, where the thick palmar skin is firmly secured by a fibrous skeleton to the palmar aponeurosis, whereas the dorsal skin is thinner and more cell, particularly throughout the joints. The characteristic furrows or creases on the elbow, wrist and the interphalangeal joints represent places of anchorage of the deep fascia. Reaching out to catch a flying object, corresponding to a cricket ball, requires the coordination and built-in motion of each muscle group within the upper limb, and indeed past. The muscles of the higher limb could additionally be grouped based on their origin and the joints on which they act: (1) Muscles arising from the axial skeleton to act on the scapula embrace trapezius, levator scapulae, the rhomboids and serratus anterior. They include supra and infraspinatus, subscapu laris, teres main and minor, and coracobrachialis. Deltoid and the clavicular head of pectoralis main additionally belong right here, even though they arise partly from the clavicle. The unopposed action of flexor pollicis longus results in the nearly ineffective thumb in palm posture. Extensor digitorum alone extends the metacarpophalangeal joints; the long flexors alone flex the interphalangeal joints. The interosseous muscles appearing with the lumbricals flex, abduct and adduct the metacarpophalangeal joints and, along side the long flexor and extensor muscular tissues, allow full extension of the proxi mal interphalangeal joints. Abductor and opponens digiti minimi and flexor digiti minimi brevis form the hypothenar eminence and act on the little finger. Many muscular tissues act on multiple joint; thus, the lengthy heads of biceps and triceps flex and prolong the glenohumeral joint, in addition to the elbow. Extensor carpi radialis longus not solely extends the wrist, but also is a robust abductor of that joint and a flexor of the elbow. Flexor carpi ulnaris is the most powerful muscle within the forearm; it contributes to elbow flexion, flexes and adducts the wrist, and is active in all sus tained movements of the wrist. The artery is described in three components which are suc cessively anterior, deep and lateral to scalenus anterior. The second and third parts are in shut relation to the primary ventral rami of C7, C8 and T1, and to the center and decrease trunks of the brachial plexus. The subclavian artery becomes the axillary artery at the posterior margin of the first rib. The axillary artery is intently related to the divisions of the brachial plexus deep to the clavicle, and to the cords beneath it. It con tinues deep to pectoralis minor and turns into the brachial artery on the inferior margin of teres major. The brachial artery is closely associated to the median nerve; each transfer from the medial side of the arm to the anterior aspect of the elbow, lying medial to the tendon of biceps brachii and deep to the bicipital aponeurosis. The widespread interosseous artery arises close to its origin and subse quently divides into the anterior and posterior interosseous arteries. The posterior interosseous artery is separated from the membrane by the deep extensor muscle tissue. At the wrist, the radial artery passes dorsally and crosses the scaphoid and trapezium. Important branches from the primary axial vessels form in depth anas tomoses that provide a collateral circulation. For example, the collateral circulation fashioned by branches of the thyrocervical trunk with the cir cumflex humeral and subscapular arteries permits survival of the limb vascular supply and lymphatic drainage after occlusion of both the third a half of the subclavian artery, or of the axillary artery deep to the clavicle and pectoralis minor.
Order 100 mg lady era with amex
The internal floor of the squamous part is divided into four deep fossae by an irregular inside occipital protuberance and by ridged sagittal and horizontal extensions from the protuberance menstrual gas and bloating lady era 100 mg order with visa. The two superior fossae are triangular and adapted to the occipital poles of the cerebral hemispheres; the inferior fossae are quadrilateral and shaped to accommodate the cerebellar hemispheres history of women's health issues lady era 100 mg cheap with visa. A broad groove with raised banks, the superior sagittal sulcus, ascends from the protuberance to the superior angle of the squamous half. A outstanding inner occipital crest descends from the protuberance and bifurcates near the foramen magnum, and provides an attachment for the falx cerebelli. On each side, a wide sulcus for the transverse sinus extends laterally from the internal occipital protuberance; the tentorium cerebelli is attached to the margins of those sulci. The proper sulcus is usually larger than the left, and passes into the sulcus for the superior sagittal sinus, whereas the left normally receives the straight sinus. The position of the confluence of the sinuses is indicated by a depression on one facet of the protuberance. The place of the fetal posterior fontanelle coincides with the junction between the superior angle of the squamous part of the occipital bone and the occipital angle of the parietal bone on either aspect. The lateral angles of the squamous part are marked internally by the ends of the transverse sulci and project between the parietal and temporal bones. The lambdoid borders prolong from superior to lateral angles and are serrated for articulation with the occipital borders of the parietal bones at the lambdoid suture. The mastoid borders extend from the lateral angles to the jugular processes, articulating with the mastoid elements of the temporal bones. Trapezius attaches to the medial third of the superior nuchal line and to the exterior occipital protuberance. Sternocleidomastoid attaches to the lateral half of the superior nuchal line, with splenius capitis just under the lateral third of that line. Thoracolumbar fascia, middle layer Erector spinae Lateral raphe Thoracolumbar fascia, anterior layer Latissimus dorsi Quadratus lumborum Iliacus Anterior superior iliac backbone Psoas main Transversus abdominis Psoas sheath Internal oblique External indirect the medial part of the area between the superior and inferior nuchal lines; obliquus capitis superior attaches to the lateral part of this space. Rectus capitis posterior major attaches to the lateral a half of the inferior nuchal line and to the bone instantly under, and rectus capitis posterior minor attaches to the medial part of the inferior nuchal line and to the bone between that line and the foramen magnum. This plate has absolutely ossified by the twenty-fifth year, at which time the occipital and sphenoid bones are fused. The inferior floor bears a small pharyngeal tubercle, about 1 cm in front of the foramen magnum, which gives attachment to the fibrous pharyngeal raphe. A small depression immediately anterior to the occipital condyle might often be replaced by a small precondylar tubercle. The anterior atlanto-occipital membrane is attached to the anterior margin of the foramen magnum. The superior surface has the form of a broad groove that slopes upwards and forwards from the foramen magnum, immediately into the basilar part of the sphenoid; together, these bones type the clivus. It could also be partly or wholly divided by a spicule of bone and transmits the hypoglossal nerve and a meningeal department of the ascending pharyngeal artery. A condylar fossa, behind every condyle, matches the posterior margin of the superior facet of the atlas vertebra in full extension of the skull. Its flooring is typically perforated by a posterior condylar canal for a sigmoid emissary vein. A quadrilateral plate, the jugular process, projects laterally from the posterior half of every condyle, and contributes the posterior a part of the jugular foramen. The jugular process is indented in entrance by a jugular notch, which may be partly divided by a small intrajugular course of projecting anterolaterally. A paramastoid course of generally tasks downwards and should even articulate with the transverse process of the atlas vertebra. An oval jugular tubercle overlies the hypoglossal canal on the superior floor of the occipital condyle. Its posterior part usually bears a shallow furrow for the glossopharyngeal, vagus and accent nerves. A deep groove containing the top of the sigmoid sinus curves anteromedially around a hook-shaped process to end at the jugular notch. The posterior condylar canal opens into the posterior cranial fossa close to the medial end of the groove. Ossification Above the best nuchal strains, the squamous a half of the occipital bone is developed in a fibrous membrane and is ossified from two centres (one on each side) from in regards to the second fetal month. Below the highest nuchal traces, the squamous part ossifies from two centres that seem in about the seventh week and shortly unite. The two components of the squamous half unite in the third postnatal month but the line of their union is recognizable at birth. The remainder of the cartilage of the occipital bone is ossified from five centres: two each for the lateral components seem through the eighth week, and one for the basilar half appears around the sixth week. Lateral(condylar)parts the lateral (condylar) components of the occipital bone flank the foramen magnum. On their inferior surfaces are occipital condyles for articulation with the superior articular facets of the atlas vertebra. They are occasionally constricted and a condyle may be in two elements (as will be the reciprocal surfaces of the atlas vertebra). Key: 1, highest nuchal line; 2, superior nuchal line; three, inferior nuchal line; 4, hypoglossal canal; 5, occipital condyle; 6, exterior occipital protuberance; 7, lambdoid margin; eight, squamous part; 9, exterior occipital crest; 10, condylar canal; eleven, foramen magnum. The lateral elements fuse with the basilar half throughout years three and 4, but fusion may be delayed till the seventh yr. A sequence of paired lateral intervertebral foramina transmits the spinal nerves and their related vessels between adjacent vertebrae. The linkages between the vertebrae include cartilaginous interbody joints and paired synovial facet (zygapophysial) joints, together with a posh of ligaments and overlying muscles and fasciae. The muscles instantly concerned with vertebral actions and hooked up to the column lie mainly posteriorly. Several large muscular tissues producing main spinal movements lie distant from the column and without direct attachment to it. The column as a whole receives its vascular provide and innervation in accordance with general anatomical principles, that are thought-about under. Vertebral column morphology is influenced externally by mechanical and environmental components and internally by genetic, metabolic and hormonal components. These all have an result on its capability to react to the dynamic forces of everyday life, corresponding to compression, traction and shear. These dynamic forces can vary in magnitude and are much influenced by occupation, locomotion and posture. Each presacral section (except the primary two cervical) is separated from its neighbour by a fibrocartilaginous intervertebral disc. Approximately 8% of general physique size is accounted for by the cervical spine, 20% by the thoracic, 12% by the lumbar and 8% by the sacrococcygeal areas. Although the usual number of vertebrae is 7 cervical, 12 thoracic, 5 lumbar, 5 sacral and four coccygeal, this complete is topic to frequent variability, and there have been reports of variation between 32 and 35 bones.
Purchase 100 mg lady era overnight delivery
The posterior superior alveolar nerve leaves the maxillary nerve in the pterygopalatine fossa women's health clinic in midland tx 100 mg lady era cheap overnight delivery. Greater (descending) palatine artery the greater palatine artery leaves the pterygopalatine fossa by way of the larger (anterior) palatine canal women's health clinic lawrenceburg tn discount 100 mg lady era overnight delivery, inside which it gives off two or three lesser palatine arteries. The greater palatine artery provides the inferior meatus of the nose, then passes on to the roof of the hard palate at the larger (anterior) palatine foramen and runs forwards to supply the hard palate and the palatal gingivae of the maxillary tooth. It gives off a branch that runs up into the incisive canal to anastomose with the nasopalatine artery, and so contribute to the arterial supply of the nasal septum. The lesser palatine arteries emerge on to the palate through the lesser (posterior) palatine foramen, or foramina, and supply the taste bud. Infraorbital nerve the infraorbital nerve could be considered the terminal branch of the maxillary nerve. It leaves the pterygopalatine fossa to enter the orbit at the inferior orbital fissure, and its subsequent course and distribution are described on page 502. Orbital branches Sphenopalatine artery the sphenopalatine artery and the higher palatine artery are the terminal branches of the maxillary artery. The sphenopalatine artery is the principal artery supplying the mucosa of the nose. It enters the nasal cavity through the sphenopalatine foramen posterior to the superior meatus. From right here, its posterior lateral nasal branches ramify over the conchae and meatuses, anastomosing with the ethmoidal arteries and nasal branches of the greater palatine artery to supply the frontal, maxillary, ethmoidal and sphenoidal air sinuses. Fine orbital branches enter the orbit via the inferior orbital fissure and supply orbital periosteum. Some fibres additionally cross by way of the posterior ethmoidal foramen to provide the sphenoidal and ethmoidal sinuses. Nasopalatine nerve Spatial arrangement of the neurovascular contents in the pterygopalatine fossa the maxillary artery and its branches are located in a plane anterior to the maxillary nerve, pterygopalatine ganglion and the nerve of the pterygoid canal. This spatial arrangement is particularly related in endoscopic approaches to the pterygopalatine fossa (Video 32. The veins accompanying the third (pterygopalatine) a half of the maxillary artery, in widespread with these accompanying the second (pterygoid) part, are within the form of a venous plexus. The nasopalatine nerve leaves the pterygopalatine fossa by way of the sphenopalatine foramen and enters the nasal cavity. When an anterior and a posterior incisive foramen exist on this fossa, the left nasopalatine nerve passes through the anterior foramen, and the right nerve passes via the posterior foramen. The nasopalatine nerve provides the lower a part of the nasal septum and the anterior a half of the onerous palate, where it communicates with the greater palatine nerve. The nasopalatine artery, a branch of the maxillary artery, accompanies the nasopalatine nerve, ending in the incisive canal, where it anastomoses with greater palatine artery and the septal department of the superior labial artery. It leaves the cranium by way of the foramen rotundum and enters the higher part of the pterygopalatine fossa, from which all its extracranial branches are derived. Crossing the pterygopalatine fossa, the nerve offers off two massive ganglionic branches that comprise fibres destined for the nostril, palate and pharynx, and these move via the pterygopalatine ganglion without synapsing. It then inclines sharply laterally on the posterior floor of the orbital process of the palatine bone and on the higher part of the posterior surface of the maxilla in the inferior orbital fissure (which is continuous posteriorly with the pterygopalatine fossa); it lies outside the orbital periosteum, and offers off its zygomatic and then posterior superior alveolar branches. About midway between the orbital apex and the orbital rim, the maxillary nerve turns medially to enter the infraorbital canal because the infraorbital nerve. The posterior superior alveolar nerves enter the back of the nasal cavity by way of the sphenopalatine foramen. Lateral posterior superior nasal nerves (about six) innervate the mucosa lining the posterior a half of the superior and middle nasal conchae and the posterior ethmoidal sinuses. Two or three medial posterior superior nasal nerves cross the nasal roof below the opening of the sphenoidal sinus to provide the mucosa of the posterior part of the roof and of the nasal septum. Palatine nerves (greater and lesser) the higher and lesser palatine nerves cross downwards from the pterygopalatine ganglion through the greater palatine canal. The greater palatine nerve descends by way of the larger palatine canal, emerges on the onerous palate from the higher palatine foramen and runs forwards in a groove on the inferior floor of the bony palate almost to the incisor enamel. It supplies the gingivae, mucosa and glands of the exhausting palate and in addition communicates with the terminal filaments of the nasopalatine nerve. Albeit small and tough to reveal angiographically, these vascular connections may however provide the arterial provide for arteriovenous malformations, dural-based fistulae and cranium base tumours, and may also compensate for occlusion of the internal carotid artery. They additionally pose a risk of inadvertent embolization of the brain parenchyma during interventional angiography of the exterior carotid artery system. In view of the extensive communications between the artery of the pterygoid canal and the extremely vascular nasopharyngeal mucosa, for example, embolization of the external carotid artery branches might end in incomplete obliteration of a vascular nasopharyngeal lesion when the artery of the pterygoid canal arises from the internal carotid artery. As the larger palatine artery runs the size of the hard palate, it permits axial mucoperiosteal flaps to be raised, if necessary bilaterally, for the reconstruction of native defects. It is also potential to pedicle the whole mucoperiosteum of the onerous palate on a single greater palatine artery. The vascular provide to the denuded palatal bone is adequate, presumably from its nasal floor, to allow regeneration of the palatal gentle tissue. Ligation of the sphenopalatine artery could also be essential in the management of refractory epistaxis. It is normally positioned endoscopically at the posterior/inferior end of the middle turbinate. The sphenopalatine artery offers the axial blood supply to the nasal septal mucosal flap (nasoseptal flap) utilized in endoscopic skull-base restore, a mirrored image of its contribution to the vascular supply to the nasal cavity (Hadad et al 2006). The ascending pharyngeal artery provides a collateral blood circulate to the petrous inside carotid artery by way of the artery of the pterygoid canal (arrow). Vidian artery as a collateral channel between the external and occluded internal carotid arteries. The trigeminal ganglion has been lifted forwards out of the trigeminal impression. The lesser (middle and posterior) palatine nerves are a lot smaller than the greater palatine nerve. They descend by way of the higher palatine canal, from which they diverge low all the way down to emerge by way of the lesser palatine foramina within the tubercle or pyramidal process of the palatine bone. Fibres conveying style impulses from the palate in all probability pass through the palatine nerves to the pterygopalatine ganglion. They pass by way of the ganglion with out synapsing and leave via the larger petrosal nerve. Their cell bodies are situated in the facial ganglion and their central processes pass via the sensory root of the facial nerve (nervus intermedius) to the gustatory nucleus in the nucleus of the tractus solitarius. Pharyngeal nerve the pharyngeal department of the maxillary nerve leaves the pterygopalatine ganglion posteriorly. It passes through the palatovaginal canal with the pharyngeal department of the maxillary artery and supplies the mucosa of the nasopharynx behind the pharyngotympanic tube. Infratemporal and pterygopalatine fossae and temporomandibular joint Extensive anastomoses, which may be sensory-to-sensory, sensory-tomotor or motor-to-motor, exist between the lower cranial nerves and higher cervical nerves. Connections between the zygomaticotemporal branch of the maxillary nerve and the temporal branches of the facial nerve, and the zygomaticofacial department of the maxillary nerve and the zygomatic branches of the facial nerve have been demonstrated (Shoja et al 2014). The connection between the zygomaticotemporal and lacrimal nerves within the orbit offering parasympathetic secretomotor fibres to the lacrimal gland, as was once thought, is less sure.
Cheap lady era 100 mg with visa
The facial surface of the maxilla forms its anterior wall breast cancer 2020 100 mg lady era order with mastercard, and is grooved internally by a delicate canal (canalis sinuosus) that homes the anterior superior alveolar nerve and vessels as they move forwards from the infraorbital canal pregnancy 0-0-1-0 100 mg lady era discount with mastercard. The posterior wall is shaped by the infratemporal floor of the maxilla; it accommodates alveolar canals that may produce ridges within the sinus and that additionally conduct the posterior superior alveolar vessels and nerves to the molar enamel. The ostium normally opens into the inferior a part of the ethmoidal infundibulum, and thence into the center meatus, through the hiatus semilunaris (the hiatus forms the area above the superior fringe of the uncinate process). All of the openings are nearer the roof than the floor of the sinus, which means that the natural drainage of the maxillary sinus is reliant on an intact mucociliary escalator; the cilia of the sinus mucoperiosteum normally beat in path of the ostium. The maxillary sinus may be incompletely divided by septa; complete septa are very rare. The thinness of its partitions is clinically important in determining the spread of tumours from the maxillary sinus. A tumour might push up the orbital ground and displace the eyeball; project into the nasal cavity, causing nasal obstruction and bleeding; protrude on to the cheek, causing swelling and numbness if the infraorbital nerve is broken; unfold again into the infratemporal fossa, causing restriction of mouth opening because of pterygoid muscle harm and ache; or unfold down into the mouth, loosening enamel and causing malocclusion. Extraction of molar teeth might harm the floor, and impact may fracture its partitions. An extraosseous anastomosis incessantly exists between the posterior superior alveolar artery and the infraorbital artery. The intra- and extraosseous anastomoses type a double arterial arcade that provides the lateral antral wall and, partly, the alveolar process. Veins corresponding to the arteries drain into the facial vein or pterygoid venous plexus on both aspect. The sinuses are innervated by the infraorbital and anterior, middle and posterior superior alveolar branches of the maxillary nerves (general sensation), and nasal branches of the pterygopalatine ganglia (parasympathetic secretomotor fibres). In the pre-antibiotic era, it was usually related to mortality from meningitis and brain abscess. Paranasal sinus an infection has the potential to spread to the orbit, cavernous sinuses, meninges and brain. The capacity to overcome infection at this site is dependent upon the virulence of the infecting organism, the pace with which applicable treatment is delivered, innate immunity and individual anatomical aspects of the sinuses that may predispose to spread of infection. Normal mucociliary clearance of the nasal and paranasal mucosa turns into paralysed or uncoordinated in a quick time with the onset of an infection and patent or probably patent drainage pathways become paramount. The center meatus types the common drainage pathway for the anterior ethmoidal, frontal and maxillary sinuses. The posterior ethmoidal and sphenoidal sinuses drain into the superior meatus and sphenoethmoidal recess. Endoscopic examination will often show infected mucus draining from these areas on this scenario (Simmen and Jones 2005). The bony walls of the sinuses are paper-thin in places and dehiscences of them, significantly of the lamina papyracea and cribriform plate of the ethmoids, the lateral wall of the sphenoid, and the orbital and posterior partitions of the frontal sinus, bring contaminated sinus mucosa into direct contact with orbital periosteum, the dura of the anterior cranial fossa and the cavernous sinus. Septic thrombophlebitis then develops and infection spreads quickly by this route. Sequelae can include blindness, intra- and extradural collections, cavernous sinus thrombosis, meningitis, frontal lobe abscess and osteomyelitis of the cranial vault if diploic veins are involved. The complicated is the frequent pathway for drainage of secretions from the maxillary and anterior group of ethmoidal sinuses; where the uncinate process attaches to the lateral nasal wall, the advanced also drains the frontal sinus. Vascular provide, lymphatic drainage and innervation the arterial provide of the maxilla is derived primarily from the maxillary arteries through the anterior, center and posterior superior alveolar branches and from the infraorbital and higher palatine arteries. C, An endoscopic view of the nostril displaying the middle turbinate and the pneumatized uncinate course of in the center meatus. D, An endoscopic view of the nose demonstrating a deviated nasal septum making contact with the left inferior turbinate. B, An endoscopic view of a right Onodi cell; the optic nerve is visible in the posterolateral wall of the cell. Medial rectus (purple arrow); inferior turbinate (yellow arrow); anterior ethmoidal air cells (green arrow). Abbreviations: C, concha bullosa (pneumatized middle turbinate); M, maxillary sinus; O, olfactory cleft; S, nasal septum. A evaluation of serial cadaveric sections in three planes, analysed with specific consideration to the anatomy of the paranasal sinuses because it pertains to endoscopic sinus surgical procedure. The 2004 Nobel Prize in Physiology or Medicine was awarded to Axel and Buck for his or her discoveries of the genetic determinants of the olfactory receptors and the group of the olfactory system in people. A discussion of the restrictions of the current nomenclature for the anatomy of the exterior nose, with recommendations for an improved terminology. A re-evaluation of the anatomical phrases in widespread utilization by endoscopic sinus surgeons and comparability with Terminologia Anatomica. A classification of the subcutaneous tissue of the external nose is included in this discussion of surgical anatomy. Simmen D, Jones N 2005 Manual of Endoscopic Sinus Surgery and its Extended Applications. Becker S 1994 Applied anatomy of the paranasal sinuses with emphasis on endoscopic sinus surgery. Boyce J, Eccles R 2006 Do changes in nasal airflow have any physiological or pathological effect on the nose and paranasal sinuses Buck L, Axel R 1991 A novel multigene family could encode odorant receptors: a molecular foundation for odor recognition. Huizing E 2003 Incorrect terminology in nasal anatomy and surgery, recommendations for improvement. A study that characterizes the normal ultrastructure of human nasal mucosa, emphasizing the differences between olfactory and respiratory epithelia. Jankowski R 2013 the Evo-Devo Origin of the Nose, Anterior Skull Base and Midface. Kuhn F 2002 Lateral Nasal Wall and Sinus Surgical Anatomy: Contemporary Understanding. American Academy of Otolaryngology/Head and Neck Surgery Foundation; Dubuque: Kendall/Hunt Publishing Company; pp. A research with the emphasis on exact measurements between surgical landmarks, with software to surgical procedures. Ruf S, Pancherz H 1996 Development of the frontal sinus in relation to somatic and skeletal maturity. A description of the vascular anatomy of the nasal cavity and the surgical approaches to management epistaxis. A consensus on the popular modern utilization of potentially confusing or ambiguous phrases in sinus anatomy. Wolf G, Anderhuber W, Kuhn F 1993 Development of the paranasal sinuses in kids: implications for paranasal sinus surgery. It extends from the cranial base to the decrease border of the cricoid cartilage (the stage of the sixth or seventh cervical verte bra), where it becomes continuous with the oesophagus. The muscular tissues of the pharynx are three round constrictors and three longitudinal elevators. The constrictors may be thought of as three overlapping cones that come up from buildings at the sides of the head and neck, and move posteriorly to insert into a midline fibrous band, the pharyngeal raphe.
Lady era 100 mg purchase mastercard
A department from the cervical plexus (C3 the women's health big book of exercises review lady era 100 mg discount visa, 4) joins the nerve just above the clavicle breast cancer t shirts lady era 100 mg purchase with amex. Intraopera tive stimulation of this department not often evokes a muscular response; it probably conveys afferent fibres from the middle and decrease components of trapezius. The nerve now turns medially, continuing in parallel to the spine of the scapula about four cm above it. At the medial end of the backbone, the nerve turns caudally once more, passing down parallel to the medial border of the scapula. It divides into terminal muscular branches about 7 cm distal to the scapular spine. Although sternocleidomastoid, and the center and the decrease parts of trapezius, could also be partially sup plied by branches from the cervical plexus, the upper a half of trapezius is innervated solely by the accessory nerve. The muscular branches from the rami be a part of deep to scalenus medius, and the trunk passes down posterolateral to the muscle, on the floor of the posterior triangle deep to the suprascapular nerve. The nerve follows a sinuous course deep to the investing fascia masking the anterior faces of the digitations of serratus anterior. It is accompa nied here by a branch of the thoracodorsal artery, and tendencies postero laterally towards the midaxillary line. Trunks of the brachial plexus Suprascapular nerve the suprascapular nerve (C5, 6) usually arises as the primary branch of the upper trunk but it incessantly springs instantly from the ventral major ramus of C5. Nerve to subclavius the slender nerve to subclavius (C5, 6) springs from the higher trunk and passes anteriorly. It descends anterior to the plexus and the subcla vian artery and passes above the subclavian vein to provide subclavius. A department from C4 to C5, which contributes to the innerva tion of the glenohumeral and elbow flexor muscular tissues, is seen often the upper trunk is formed by C5 and C6, the place these nerves emerge from deep to scalenus anterior. The decrease trunk is fashioned by C8 and T1, where these nerves cross anterior to the primary rib. The ramus of T1 takes an upward course across the deep face of the neck of the first rib behind the pleura and the vertebral and subclavian arteries in the path of the decrease trunk. The forma tion of the trunks is pretty consistent; they lie in front of one another quite than side by side, with the subclavian artery passing anteromedi ally. The phrenic nerve crosses C5 to move anteromedially on the floor of scalenus anterior. The upper trunk, its divisions and the suprascapu lar nerve can all be palpated in the supraclavicular fossa in a subject of regular physique. The inspecting finger identifies first the subclavian pulse and then the nerves, whilst rolling the fingertip laterally (see Video forty six. Divisions of the brachial plexus the trunks divide into anterior and posterior divisions. The upper trunk divides 2�3 cm above the clavicle, and the divisions of the center and lower trunk are shaped deep to the clavicle. It passes posteriorly, pier cing scalenus medius, to run down within the plane between levator scapu lae and serratus posterior superior and the posterior scalene muscular tissues. The dorsal scapular nerve inside vates the rhomboid muscle tissue and, together with branches from C3 and C4, it supplies levator scapulae. BloodsupplyThe blood provide of the brachial plexus is derived from vessels arising from the subclavian and vertebral arteries. Important branches pass from the vertebral artery to the rami of C5 and C6 and the more proximal cervical nerves. Extensive contributions come from the suprascapular and superficial cervical arteries that arise from the thyrocervical trunk. In at least onethird of cases, the superficial cervical and dorsal scapular arteries come up from the thyrocervical trunk because the transverse cervical artery. In clinical phrases, the arteries arising from the thyrocervical trunk have turn into the lifeline to the higher limb and should be preserved throughout operations in cases when the ruptured subclavian artery has not been repaired. The dorsal scapular artery may arise from the third part of the subclavian artery to move between the upper and middle trunks of the brachial plexus. The rami enter the posterior triangle of the neck between scalenus anterior and medius. Rami from C7 and C8 are the largest (C8 incorporates about 30,000 myeli nated axons) and those from C5 and T1 are the smallest (between 15,000 and 20,000 myelinated axons). An adult brachial plexus con tains between one hundred twenty,000 and a hundred and fifty,000 myelinated axons, of which 25% innervate the shoulder girdle and glenohumeral joint. The proportion of motor fibres is biggest in C5 and C8; the sensory contribution is biggest in C7. A complex interchange of branches, before the principle nerves of the higher limb are fashioned, produces the trunks, divisions and cords of the brachial plexus. Note the sequence: ventral (anterior) major rami; trunks; divisions; cords; nerves. The trunks are upper, middle and lower, and the cords are lateral, medial and posterior, according to their place in relation to the axillary artery, which is variable. The posterior division of the decrease trunk is persistently smaller than the anterior division and is absent in about 10% of circumstances. Cords of the brachial plexus 782 the cords are shaped by the confluence of divisions: the lateral twine from the anterior divisions of the upper and middle trunks; the pos terior twine by all three posterior divisions; and the medial twine by the anterior division of the lower trunk and, typically, by a department from the anterior division of the center trunks. The divisions of the trunks and the formation of the cords characterize an necessary anatomical and practical differentiation. The posterior divisions and posterior wire innervate postaxial (extensor) musculature; the anterior divisions and the lateral and medial cords innervate preaxial (flexor) musculature. The formation and relations of the three cords are variable and, indeed, their designations considerably misleading. Immediately inferior to the clavicle, the posterior wire is lateral, the medial wire is posterior, and the lateral twine is anterior, in relation to the axillary artery; the cords assume their acceptable relations about the axillary artery deep to pectoralis minor. There is considerable variation in this association; mostly, the axillary artery lies anterior to the three cords and the median nerve. The branches of the posterior wire, the largest of the three trunks, are constant. The branches of the medial cord are normally predictable; the medial pectoral nerve and medial cutaneous nerve of the forearm are succeeded by the division into the medial root of the median nerve and the ulnar nerve. The greatest variation in for mation of trunk nerves is found throughout the lateral wire. Occasionally, the musculocutaneous nerve arises extra distally than traditional, springing both immediately from the lateral wire as two or three branches or even from the median nerve itself. Sometimes, the best of these branches enters coracobrachialis no extra than 2 or three cm below the coracoid process.
Lady era 100 mg otc
Other extensions of the fascia bulbi cross medially and laterally pregnancy stages 100 mg lady era order with mastercard, and attach to the orbital walls women's health clinic grafton lady era 100 mg buy generic on-line, forming the transverse ligament of the attention. This structure is of uncertain significance, but presumably plays a component in drawing the fornix upwards in gaze elevation and may act as a fulcrum for levator actions. Other numerous finer fasciae type radial septa that stretch from the fascia bulbi and the muscle sheaths to the periosteum of the orbit, and so provide compartments for orbital fat. It additionally attaches to the trochlea and, because the lacrimal fascia, types the roof and lateral wall of the fossa for the nasolacrimal sac. Orbital connective tissue pulleys There is mounting proof that challenges the normal view that the recti are hooked up solely at their origin and scleral insertion. The idea that orbital connective tissue sheaths elastically coupled to the orbital walls function as pulleys was initially proposed as an explanation for the noticed orbital stability of rectus muscle paths (Miller 1989). Each pulley consists of an encircling sleeve of collagen situated within the fascia bulbi, close to the equator of the globe. Elastic fibres and bundles of smooth muscle confer the required inside rigidity to the construction (Demer 2002). Although the unique model described a passive pulley system, the current view is that fibres from the orbital surface of the muscle insert into the pulley sleeve to enable small longitudinal actions. Fat additionally lies between the muscles and periosteum, and is restricted anteriorly by the orbital septum. Collectively, the fats helps to stabilize the place of the eyeball and likewise acts as a socket within which the attention can rotate. Abbreviations: atc, adipose tissue compartments; eb, ethmoid bone; fn, frontal nerve; frb, frontal bone; ir, inferior rectus; lps, levator palpebrae superioris; lr, lateral rectus; m, maxilla (bone); mr, medial rectus; ncn, nasociliary nerve; opn, optic nerve; som, superior indirect; sov, superior ophthalmic vein; sr, superior rectus. The palpebral apertures are widened in states of fear or excitement by contraction of the superior and inferior tarsal muscular tissues because of elevated sympathetic exercise. Levator palpebrae superioris is an elevator of the upper eyelid, and the other six, i. Complete congenital absence of the extraocular muscle tissue, thought to represent a extreme type of congenital fibrosis syndrome, has been described (Brady et al 1992). Rarely, people have deep orbital bands consistent with supernumerary extraocular muscle tissue (Khitri and Demer 2010). The tendinous ring is carefully adherent to the dural sheath of the optic nerve medially and to the encircling periosteum. Inferior rectus, part of medial rectus and the decrease fibres of lateral rectus are all hooked up to the decrease a part of the ring, whereas superior rectus, part of medial rectus and the upper fibres of lateral rectus are all hooked up to the upper part. A second small tendinous slip of lateral rectus is hooked up to the orbital floor of the larger wing of the sphenoid, lateral to the common tendinous ring. It has a brief slim tendon at its posterior attachment and broadens steadily, then extra sharply because it passes anteriorly above the eyeball. Some of its tendinous fibres cross straight into the higher eyelid to connect to the anterior surface of the tarsus, while the rest radiate and pierce orbicularis oculi to move to the skin of the higher eyelid. Where the two muscle tissue separate to attain their anterior attachments, the fascia between them varieties a thick mass to which the superior conjunctival fornix is hooked up; this is usually described as a further attachment of levator palpebrae superioris. Traced laterally, the aponeurosis of the levator passes between the orbital and palpebral components of the lacrimal gland to connect to the orbital tubercle of the zygomatic bone. Traced medially, it loses its tendinous nature because it passes carefully over the reflected tendon of superior indirect, and continues on to the medial palpebral ligament as loose strands of connective tissue. Innervation Levator palpebrae superioris is innervated by a branch of the superior division of the oculomotor nerve that enters the inferior floor of the muscle. Sympathetic fibres to the graceful muscle component of levator palpebrae superioris (superior tarsal muscle) are derived from the plexus surrounding the internal carotid artery; these nerve fibres may be a part of the oculomotor nerve within the cavernous sinus and move forwards in its superior department. Superior rectus Levator palpebrae superioris Orbital apex Actions Levator palpebrae superioris elevates the upper eyelid. During this course of, the lateral and medial components of its aponeurosis are stretched and thus limit its motion; the elevation can additionally be checked by the orbital septum. Levator palpebrae superioris is linked to superior rectus by a examine ligament; thus the higher eyelid elevates when the gaze of the attention is directed upwards. The position of the eyelids is determined by reciprocal tone in orbicularis oculi and levator palpebrae superioris, and on the diploma of ocular protrusion. In the opened position, the higher eyelid covers the higher part of the cornea, while the lower lid lies just under its lower margin. The eyes are closed by movements of each lids, produced by the contraction of the palpebral part of orbicularis oculi and rest of levator palpebrae superioris. In wanting upwards, the levator contracts and the upper lid follows the ocular movement. At the same time, the eyebrows are additionally often raised by the frontal parts of occipitofrontalis to diminish their overhang. The decrease lid lags behind ocular motion, in order that more sclera is uncovered beneath the cornea and the lid is bulged a little by the decrease part of the elevated eye. When the attention is depressed, each lids move; the higher retains its regular relation to the eyeball and still covers a few quarter of the cornea, whereas the lower lid is depressed because the extension of the thickened fascia of inferior rectus and inferior oblique pull on its tarsus as the former contracts. Extraocular muscles Each rectus muscle passes forwards, in the place implied by its name, to be hooked up anteriorly by a tendinous enlargement into the sclera, posterior to the margin of the cornea. However, before their scleral attachment, the recti make functionally essential connections inside orbital connective tissue that influence muscle motion. Superior rectus Vascular supply Lateral rectus receives its arterial supply from the ophthalmic artery immediately and/or from its lacrimal branch. Innervation Lateral rectus is innervated by the abducens nerve by branches that enter the medial surface of the muscle. It arises from the higher part of the widespread tendinous ring, above and lateral to the optic canal. The insertion is slightly indirect, the medial margin more anterior than the lateral margin. The tendon subsequently descends posterolaterally and inferior to superior rectus, and is hooked up to the sclera in the superolateral part of the posterior quadrant behind the equator, between the superior and lateral recti. Vascular supply Superior rectus receives its arterial provide both immediately from the ophthalmic artery and indirectly from its supraorbital branch. Innervation Superior rectus is innervated by the superior division of the oculomotor nerve that enters the inferior surface of the muscle. Actions Superior rectus strikes the attention so that the cornea is directed upwards (elevation) and medially (adduction). Because a check ligament extends from superior rectus to levator palpebrae superioris, elevation of the attention additionally results in elevation of the upper eyelid. Vascular supply Superior oblique receives its arterial supply immediately from the ophthalmic artery and indirectly from its supraorbital branch. Inferior rectus Inferior rectus arises from the widespread tendinous ring, under the optic canal. Innervation Superior indirect is innervated by the trochlear nerve, which enters the superior floor of the muscle.
Diseases
- Methylcobalamin deficiency cbl G type
- Chromosome 22 trisomy mosaic
- Infantile spasms
- Olivopontocerebellar atrophy type 1
- Enchondromatosis dwarfism deafness
- Fetal minoxidil syndrome
Buy lady era 100 mg mastercard
The ascending pharyngeal artery is crossed by styloglos sus and stylopharyngeus pregnancy 11 weeks lady era 100 mg purchase otc, and longus capitis lies posterior to it women's health clinic elizabeth buy lady era 100 mg mastercard. It provides off quite a few small branches to supply longus capitis and longus colli, the sympathetic trunk, the hypoglossal, glossopharyngeal and vagus nerves, and some of the cervical lymph nodes. It anastomoses with the ascending palatine department of the facial artery and the ascending cervical branch of the vertebral artery. Pharyngeal artery the pharyngeal artery gives off three or four branches to supply the constrictor muscles of the pharynx and stylo pharyngeus. A variable ramus supplies the palate, and may replace the ascending palatine department of the facial artery. The artery descends for wards between the superior border of the superior constrictor and levator veli palatini to the taste bud, and likewise supplies a department to the palatine tonsil and the pharyngotympanic tube. It descends along the lateral border of thyrohyoid to reach the apex of the lobe of the thyroid gland. Lying medially are the inferior constrictor muscle and the exterior laryngeal nerve; the nerve is often posteromedial, and due to this fact in danger when the artery is being ligated. Meningeal branches the meningeal branches are small vessels that provide the nerves that traverse the foramen lacerum, jugular foramen and hypoglossal canal, and the related dura mater and adjoining bone. One department, the posterior meningeal artery, reaches the cerebellar fossa via the jugular foramen, and is normally thought to be the terminal department of the ascending pharyngeal artery. Lingual artery Ascending palatine artery the ascending palatine artery arises near the origin of the facial artery. It passes up between styloglossus and stylopharyngeus to attain the facet of the pharynx, along which it ascends between the superior constrictor of the pharynx and medial pterygoid in course of the cranial base. One department follows this muscle, winding over the higher border of the superior constrictor of the pharynx to provide the taste bud and to anastomose with its fellow of the other facet and the greater pala tine department of the maxillary artery. Tonsillar artery the tonsillar artery supplies the primary blood provide to the palatine tonsil. It ascends between medial pterygoid and sty loglossus, penetrates the superior constrictor of the pharynx on the higher border of styloglossus, and enters the inferior pole of the tonsil. Its branches ramify in the tonsil and in the musculature of the posterior a part of the tongue. It arises because the facial artery separates from the submandibular gland and turns forwards on mylo hyoid under the mandible. It provides the overlying skin and muscular tissues, and anastomoses with a sublingual branch of the lingual and mylo hyoid department of the inferior alveolar artery. At the chin, it ascends over the mandible, and divides into superficial and deep branches, which anastomose with the inferior labial and mental arteries to provide the chin and decrease lip. Glandular branches Three or four giant vessels provide the sub mandibular salivary gland and associated lymph nodes, adjacent muscular tissues and skin. It arises anteromedially from the exterior carotid artery opposite the tip of the greater cornu of the hyoid bone, between the superior thyroid and facial arteries. Ascending medially at first, it loops down and forwards, passes medial to the posterior border of hyoglossus and then runs horizontally forwards deep to it. The lingual artery subsequent ascends once more almost vertically, and courses sinu ously forwards on the inferior surface of the tongue so far as its tip. Skin, fascia and platysma are superficial to it, whereas the middle pharyngeal constrictor muscle is medial. The artery ascends somewhat medially, then descends to the extent of the hyoid bone, and the loop so shaped is crossed externally by the hypoglossal nerve. The second half passes alongside the upper border of the hyoid bone, deep to hyoglossus, the tendons of digastric and stylohyoid, the lower a part of the submandibular gland and the posterior part of mylohyoid. Here, its medial aspect adjoins the middle constrictor muscle and it crosses the stylohyoid ligament accompanied by lingual veins. The third part is the arteria profunda linguae, which turns upwards close to the anterior border of hyoglossus and then passes forwards close to the inferior lingual floor near the frenulum, accompanied by the lingual nerve. Genioglossus is a medial relation, and the inferior longitudinal muscle of the tongue lies lateral to it under the lingual mucous membrane. Near the tip of the tongue, the lingual artery anastomoses with its fellow of the opposite side. Occipital artery Suprahyoid artery the suprahyoid artery is a small branch that runs alongside the upper border of the hyoid bone to anastomose with the contralateral artery. Dorsal lingual arteries Sublingual artery Facial artery the dorsal lingual arteries are described on web page 513. At first on the middle pharyngeal constrictor, it may attain the lateral surface of styloglossus, separated there from the palatine tonsil solely by this muscle and the lingual fibres of the superior constric tor. Medial to the mandibular ramus, it arches upwards and grooves the posterior aspect of the submandibular gland. It then turns down and descends to the lower border of the mandible in a lateral groove on the submandibular gland, between the gland and medial pterygoid. Reach ing the floor of the mandible, the facial artery curves round its inferior border, anterior to masseter, to enter the face; its further course is described on web page 498. In the neck, this might be in order that the artery is in a position to adapt to the transfer ments of the pharynx during deglutition, and equally on the face, so that the artery can adapt to movements of the mandible, lips and cheeks. Facial artery pulsation is most palpable where the artery crosses the mandibular base, and again close to the nook of the mouth. Its branches in the neck are the ascending palatine, tonsillar, submental and glandular arteries. At its origin, the artery is crossed superficially by the hypoglossal nerve, which winds spherical it from behind. The artery subsequent passes backwards, up and deep to the posterior stomach of digastric, and crosses the inner carotid artery, internal jugular vein, and hypoglossal, vagus and accessory nerves. Between the transverse process of the atlas and the mastoid course of, the occipital artery reaches the lateral border of rectus capitis lateralis. It then runs in the occipital groove of the temporal bone, medial to the mastoid process and attachments of sternocleidomastoid, splenius capitis, longissimus capitis and digastric, and lies successively on rectus capitis lateralis, obliquus superior and semispinalis capitis. The occipital artery has two major branches (upper and lower) to the higher a part of sternocleidomastoid in the neck. The decrease department arises close to the origin of the occipital artery, and will generally come up directly from the external carotid artery. It descends backwards over the hypoglossal nerve and inner jugular vein, enters sternocleidomastoid and anastomoses with the sternocleidomastoid department of the superior thyroid artery. The upper branch arises because the occipital artery crosses the accessory nerve, and runs down and backwards superficial to the intern al jugular vein. Posterior auricular artery 454 the posterior auricular artery is a small vessel that branches posteriorly from the exterior carotid simply above digastric and stylohyoid. It ascends between the parotid gland and the styloid course of to the groove between the auricular cartilage and mastoid course of, and divides into auricular and occipital branches, which are described with the face on page 499.
Lady era 100 mg cheap without prescription
The dome projects up to pregnancy jobs 100 mg lady era buy with mastercard 8�10 mm caudal women's heart health tips lady era 100 mg buy cheap, and 3�6 mm anterior, to the anterior septal angle, the difference between the two creating the supratip break-point. Classically, transverse connective tissue fibres have been described binding the medial and intermediate crura; interdomal, intercrural and septocrural ligaments have been described. Cadaveric studies by Zhai et al (1995) disputed the presence of transverse fibres, and located that every one connective tissue fibres run parallel to the cartilages. These findings however, the fibrous connections along the length of the medial and intermediate crura form a single useful unit in the tip. It runs on the caudal edge of the alar rim in the anterior half, then moves cephalically, leaving a gentle tissue area in the rim laterally. Typically, the longitudinal axis of the lateral crus types an angle of 45� with the septum. The lateral crus might take a highly variable position, being both convex or concave, or a mixture of each, in medial and lateral parts; asymmetry from facet to facet has been reported in over half of anatomical specimens. A chain of lateral accent cartilages with dense fibrous attachments connect to the lateral crus and the piriform aperture, and to the anterior nasal spine by way of connection within the ground of the nostril. Tipsupport the inherent power and shape of the cartilaginous framework, and its attachments to surrounding buildings, provide help to the tip of the nose. Major tip assist mechanisms the most important mechanisms supporting the tip are: the dimensions, form and strength of the major alar cartilages; the medial crural footplate attachment to the caudal part of the septum; the attachment of the caudal border of the lateral cartilages to the cephalic border of the most important alar cartilages; and the cartilaginous dorsal septum. Minor tip help mechanisms the minor mechanisms supporting the tip are: the ligamentous sling spanning the domes of the lower lateral cartilages. Rhinoplasty approaches, either via an intercartilaginous incision between the lateral and the most important alar cartilages (closed rhinoplasty), or through an incision caudal to the main alar cartilages and degloving the entire cartilaginous framework (open rhinoplasty), disrupt the tip help mechanisms; the integrity of those mechanisms should be restored during the process to forestall lack of tip assist and subsequent tip ptosis. Its fibres pass to the columella, the cellular part of the nasal septum and the base of the medial crus of the nasal cartilage. Ala of vomer Vaginal process of medial pterygoid plate Vascular provide Depressor septi is provided by the superior labial department of the facial artery. Sphenoidal process of palatine bone Innervation Depressor septi is innervated by the buccal department, and generally by the zygomatic department, of the facial nerve. Actions Depressor septi pulls the columella, the tip of the nostril and the nasal septum downwards. Choanae Pterygoid hamulus Medial pterygoid plate of sphenoid Pyramidal means of palatine bone Horizontal plate of palatine bone Levator labii superioris alaeque nasi Nasal skin is innervated by the infratrochlear and exterior nasal branches of the nasociliary nerve (ophthalmic division, trigeminal nerve), and the nasal branch of the infraorbital nerve (maxillary division, trigeminal nerve). Vascular supply Levator labii superioris alaeque nasi is provided by the facial artery and the infraorbital branch of the maxillary artery. Innervation Levator labii superioris alaeque nasi is innervated by zygomatic and superior buccal branches of the facial nerve. Actions the lateral slip raises and everts the upper lip and raises, deepens and will increase the curvature of the highest of the nasolabial furrow. The nasal cavity communicates with the paranasal sinuses and opens into the nasopharynx via a pair of oval openings, the posterior nasal apertures or choanae. The parameters of the intranasal spaces depend on age and gender: progress is usually completed by the age of 16 (Samoliski et al 2007). Each half of the nasal cavity has a vestibule, roof, flooring, medial (septal) and lateral walls. They include anomalous nasi, hooked up to the frontal process of the maxilla, procerus, transverse part of nasalis and the higher lateral cartilage. It is restricted above and behind by a curved ridge, the limen nasi, raised the place the higher ala of the lateral cartilaginous crus overlaps the decrease edge of the lateral nasal cartilage on both sides. On the septal side of the nasal cavity, the superior fringe of the medial crus of the main alar cartilage (the medial intumescence) marks the boundary between the nasal vestibule and the nasal cavity. The alae and lower a part of the nasal septum are supplied by lateral nasal and septal branches of the facial artery, and the lateral features and dorsum of the nostril are equipped by the dorsal nasal department of the ophthalmic artery and the infraorbital branch of the maxillary artery. The frontomedian region of the face, including the nostril, drains to the facial vein, and the orbitopalpebral space of the face, including the foundation of the nose, drains to the ophthalmic veins. Lymph drainage is primarily to the submandibular group of nodes, though lymph draining from the root of the nose drains to superficial parotid nodes. The anterior slope is shaped by the nasal spine of the frontal bones and by the nasal bones. The central region is shaped by the cribriform plate of the ethmoid bone, which separates the nasal cavity from the floor of the anterior cranial fossa. It accommodates numerous small perforations that transmit the olfactory nerves and their ensheathing meningeal layers, and a separate anterior foramen that transmits the anterior ethmoidal nerve and vessels. The medial slip blends into the perichondrium of the lateral crus of the major alar cartilage of the nostril and the pores and skin over it. The lateral slip is prolonged into the lateral a part of the higher lip, the place it blends with levator labii superioris and orbicularis oris. Superficial fibres of the lateral slip curve laterally across the front of levator labii superioris and attach along the ground of the dermis on the higher part of the nasolabial furrow and ridge. Thus, the superficial muscular aponeurotic system is steady from the nasofrontal course of to the nasal tip, splitting at the caudal finish of the lateral cartilage into superficial and deep layers, each with medial and lateral parts (Oneal et al 1999). Dissection in rhinoplasty is normally performed in a sub-superficial muscular aponeurotic system plane. Posteriorly, the roof of the nasal cavity is formed by the anterior aspect of the body of the sphenoid, interrupted on all sides by a gap of a sphenoidal sinus, and the sphenoidal conchae or superior conchae. Anteriorly, close to the septum, a small infundibular opening in the bone of the nasal ground leads into the incisive canals that descend to the incisive fossa; this opening is marked by a slight despair in the overlying mucosa. The floor of the nose could additionally be deficient because of congenital clefting of the hard and/or taste bud. Other bones that make minor contributions to the septum on the higher and lower limits of the medial wall are the nasal bones and the nasal backbone of the frontal bones (anterosuperior), the rostrum and crest of the sphenoid (posterosuperior), and the nasal crests of the maxilla and palatine bones (inferior). The conchae have been removed to present the positions of the ostia of the paranasal sinuses and the nasolacrimal duct. Its anterosuperior margin is related above to the posterior border of the internasal suture, and the distal finish of its superior portion is steady with the higher lateral cartilages. The anteroinferior border is related by fibrous tissue on all sides to the medial crurae of the main alar cartilage. Anteroinferiorly, the cartilaginous septum is hooked up to the anterior nasal spine, which is shaped by anterior projections of each maxillary crest, and it has a strong, tongue-in-groove attachment with the premaxilla and vomer. The posterosuperior border joins the perpendicular plate of the ethmoid, while the posteroinferior border is hooked up to the vomer and, anterior to that, to the nasal crest and anterior nasal backbone of the maxilla. Above the incisive canals, at the lower edge of the septal cartilage, a melancholy pointing downwards and forwards is all that is still of the nasopalatine canal, which related the nasal and buccal cavities in early fetal life. Near this recess, a minute orifice leads again right into a blind tubule, 2�6 mm lengthy, which lies on each side of the septum and houses remnants of the vomeronasal organ (see below). It contains three projections of variable size: the inferior, center and superior nasal conchae or turbinates. The conchae curve inferomedially in general, every roofing a groove, or meatus, which is open to the nasal cavity. The main options of the lateral nasal wall are a rounded elevation, the bulla ethmoidalis, and a curved cleft, the hiatus semilunaris, formed by the posterior edge of the uncinate process and the anterior face of the ethmoidal bulla. This constitutes the medial restrict of the ethmoidal infundibulum, a slit-like space that leads in course of the maxillary ostium.
Order 100 mg lady era with visa
After a quantity of hours of normal activity pregnancy headaches lady era 100 mg cheap visa, the discs lose roughly 20% of their water and peak breast cancer apparel lady era 100 mg discount without prescription. This change makes the ligaments slack and tremendously reduces the bending stiffness of the backbone, so that comparatively more of the steadiness of the spine must then be supplied by the musculature. It is essential to recognize the method in which during which the muscles of the back work along side those of the abdominal wall, particularly the indirect and transversus muscular tissues, and with these of the lower limbs. The erector spinae group and inside oblique and transversus abdominis are anatomically and functionally related by the thoracolumbar fascia (which encloses the former, and into which the latter are inserted). This fascia, together with collagenous tissue within the again muscle tissue, performs an essential role in resisting forward bending of the trunk, and during handbook handling. The fascia is tensioned primarily by flexing the trunk, though this rigidity could also be enhanced slightly by the lateral pull of the abdominal muscle tissue. It is functionally advantageous to generate tension in the fascia and muscle sheaths because the elastic strain energy saved in these stretched tissues can be utilized to help deliver the trunk to an upright place and so cut back the metabolic value of the motion (Adams et al 2006). The thoracolumbar fascia may also have an important operate in transferring load between the trunk and the decrease limbs; tension within the fascia can be increased by the actions of gluteus maximus and the hamstrings in addition to by trunk flexion. Gravity all the time plays a part: actions with gravity normally contain the eccentric contraction of antagonists. Flexion is effected by longus capitis and longus colli, scaleni, sternocleidomastoid and rectus abdominis of both sides, aided in the lumbar area by the abdominal obliques; extension by the erector spinae complex and the transversospinalis group, splenius, semispinalis capitis and trapezius of either side, together with the suboccipital muscle tissue; lateral flexion by ipsilateral longissimus, iliocostalis, stomach obliques and flexors, and quadratus lumborum; and rotation by sternocleidomastoid, splenius cervicis, belly obliques, rotatores and multifidus. There is appreciable variation between segments of the column in phrases of stability and mobility; essentially the most cellular levels are the least steady. The latter are these in which the ratio of intervertebral disc peak to vertebral physique top is highest. Pure ligamentous/capsular accidents resulting in instability may be particularly tough to diagnose within the absence of gross radiological signs. In the cervical spine, subluxation and dislocation of the side joints generally occur with out bony harm because of the orientation of the articular sides. Acute infections, spreading locally or by way of the blood stream, might result in the Surface anatomy the diurnal expulsion of water from intervertebral discs also affects the distribution of compressive loading within the spine. As the day progresses, the hydrostatic pressure within the nucleus pulposus falls, and stress concentrations arise within the anulus fibrosus and side joints. All ligaments of the column, in addition to the side joint capsules, are necessary within the upkeep of stability. The anterior longitudinal ligament is very sturdy, and resists translational displacement (shear) of the vertebrae in addition to extension. All the ligaments of the posterior advanced resist flexion and rotation, and their integrity determines the vary of actions allowed. At the restrict of lumbar flexion, the column is supported mainly by the thoracolumbar fascia and by collagenous tissue within the electrically silent muscle tissue of the again. Movements are both determined and constrained by the form and orientation of the facet joints, whose articular surfaces stabilize the column primarily by resisting horizontal gliding (shear) actions and axial rotation. In the most mobile areas, the joint surfaces are flatter and more horizontally positioned, as will turn into obvious if a typical cervical facet joint is compared with a typical lumbar joint. Certain areas of the vertebral column are further stabilized by further extraspinal elements. The thoracic backbone is stabilized by its place as an integral part of the thoracic cage and by its sturdy ligamentous linkages with the ribs. The contribution to stability conferred by the musculature has been grossly underrated. This effect is especially marked for erector spinae, which controls global posture and movement. For most again problems in medical practice, especially chronic low again pain, enhancing muscle energy, stamina and coordination with the many other muscle teams that contribute to stability. Furthermore, neglecting the musculature may clarify the relatively excessive failure charges from surgical procedure. Mechanical harm to the vertebral column could additionally be produced by flexion, extension, distraction, rotation, shear or compression; movements that cause damage are commonly mixed. A widespread postural deviation seen all through the spine is scoliosis or lateral curvature of the spine. In structural scoliosis, the lateral curvature is related to vertebral rotation, and both the curve and the rotation turn into extra accentuated on ahead flexion. A sciatic or antalgic scoliosis is a brief deformity produced by the protective action of muscles in certain painful situations of the spine. Nachemson (1975) showed that discs were loaded maximally in sitting and in lifting in a forward-leaning place, so sitting posture and lifting have acquired appreciable ergonomic attention. In sitting, the objective has been to determine the seat kind and reclining angle associated with lowest disc strain and the least paraspinal muscle exercise. When sitting with the hips and knees flexed to 90�, the pelvis rotates posteriorly, flattening the lumbar lordosis and consequently growing the load on the intervertebral discs. The compressive force appearing on the backbone is shared between the vertebral bodies and the neural arch. In the lumbar spine, the neural arch sometimes resists 20% of this pressure once the disc height has been reduced by diurnal fluid expulsion, and when the backbone is positioned upright. However, age-related narrowing of the disc could cause greater than 50% of the compressive drive to be resisted by the neural arch, which may clarify why osteoarthritis of the side joints generally follows disc degeneration. When lifting, guide handling advisers emphasize the significance of leg lifting as opposed to back lifting. The use of deep inspiration to raise intra-abdominal stress whereas lifting has also been suggested, as this is believed to supply additional support to the lumbar spine. The spine is at risk when lifting is mixed with twisting, lateral bending and uneven postures. However, heavy lifting remains one of the key work-related risk components for the spine along with wholebody vibration, extended sitting, twisting and bending. The maintenance of fine posture is a compromise between minimizing the load on the backbone and minimizing the muscle work required. The well-balanced erect body has a line of gravity that extends from the extent of the external auditory meatus, via the dens of the axis simply anterior to the physique of the second thoracic vertebra, via the centre of the body of the twelfth thoracic vertebra, and thru the rear of the physique of the fifth lumbar vertebra to lie anterior to the sacrum. The place of the line of gravity might transfer anteriorly with locomotion and should range between individuals. The thoracic spine is held convex posteriorly, and this posture primarily outcomes from the structure of the underlying vertebrae. However, this curve or kyphosis can become exaggerated to give the impression of a rounded again. The diploma of this lordosis is set by the lumbosacral angle and is often 30�45�. The muscles answerable for this posture embrace erector spinae, rectus abdominus, the interior and external obliques, psoas major, iliacus, the gluteal and hamstring muscles. The furrow is most shallow within the decrease cervical region and is deepest in the midlumbar zone.
100 mg lady era free shipping
Otitis media Microstructure Histologically embarrassing women's health issues lady era 100 mg order line, the tympanic membrane consists of an outer cuticular layer women's health clinic minneapolis discount lady era 100 mg with mastercard, an intermediate fibrous layer and an inside mucous layer. It is keratinized, stratified squamous in type, devoid of dermal papillae and hairless. Its subepithelial tissue is vascularized and will develop a quantity of peripheral papillae. There are quite a few desmosomes between cells, the deepest of which lie on a steady basal lamina, but lack epithelial pegs and hemidesmosomes. The cells of this stratum will be inclined for lateral migration and differentiation not shared with some other stratified squamous epithelia in the body. The fibrous stratum consists of an exterior layer of radiating fibres that diverge from the handle of the malleus, and a deep layer of round fibres, that are plentiful peripherally but sparse and scattered cen- It is assumed that acute otitis media normally arises because of ascending an infection from the nasopharynx by way of the pharyngotympanic tube to the middle ear cleft. Swelling secondary to the an infection might outcome within the closure of each exits from the middle ear, i. The latter could burst, releasing mucopurulent discharge into the external acoustic meatus, which ends up in a release of the stress within the middle ear and a diminution within the ranges of pain. After a brief period, the discharge dries up and, for the most part, the resultant perforation of the tympanic membrane heals. Normal air flow and drainage of mucus from the center ear are restored as soon as the swelling and performance of the pharyngotympanic tube resolve. The immune defence system sterilizes the exudates of organisms, resulting in a sterile mucoid effusion, otitis media with effusion or glue ear (see below). The effusion could cause protracted deafness as a result of its relatively incompressible nature prevents free vibration of the tympanic membrane (Bluestone and Klein 2002). Myringoplasty Persistent perforation of the tympanic membrane attributable to infection or trauma leads to listening to impairment and predisposes to persevering with infection because of contamination with organisms from the external acoustic meatus. This situation is recognized as chronic suppurative otitis media of the tubotympanic type. Myringoplasty is a surgical procedure that uses a connective tissue scaffold or graft to help healing of the perforation. The most common technique involves the elevation of the tympanic anulus and the placement of a piece of fibrous connective tissue. A, the lateral wall and adjoining elements of the anterior and superior partitions have been removed; the facial canal and carotid canal have been opened. B, A section Mastoid cells along the axis of the petrous part of the temporal bone. The healed edges of the perforation are stripped of epithelium to encourage healing and scar formation. The fibrous tissue helps the therapeutic tympanic membrane and should, partially, be incorporated into the repair. Once the perforation is healed, the vibratory operate of the tympanic membrane is normally restored to regular. Medial wall the medial wall of the tympanic cavity is also the lateral boundary of the internal ear. The promontory is a rounded prominence furrowed by small grooves that lodge the nerves of the tympanic plexus. A minute spicule of bone frequently connects the promontory to the pyramidal eminence of the posterior wall. The apex of the cochlea lies near the medial wall of the tympanic cavity, anterior to the promontory. The fenestra vestibuli is a kidney-shaped opening located above and behind the promontory, and main from the tympanic cavity to the vestibule of the internal ear. It is occupied by the base of the stapes, the footplate; the circumference of the footplate is connected to the margin of the fenestra by an anular ligament. Occasionally, one other ridge of bone, the ponticulus, leaves the promontory above the subiculum and runs to the pyramid on the posterior wall of the cavity. The fenestra cochleae lies completely underneath the overhanging fringe of the promontory in a deep hole or niche, and is positioned very obliquely. This is somewhat concave towards the tympanic cavity and convex in the direction of the cochlea, and is bent so that its posterosuperior third varieties an angle with its anteroinferior two-thirds. The membrane consists of an exterior layer derived from the tympanic mucosa; an inner layer, derived from the cochlear lining membrane; and an intermediate, fibrous layer. The prominence of the facial nerve canal indicates the place of the upper a part of the bony facial canal (Fallopian canal), which accommodates the facial nerve. The canal crosses the medial tympanic wall from the cochleariform course of anteriorly, runs just above the fenestra vestibuli, after which curves down into the posterior wall of the cavity. Posterior wall the posterior wall of the tympanic cavity is wider above than under. The aditus to the mastoid antrum is a large irregular aperture that leads back from the epitympanic recess into the higher a half of the mastoid antrum. A rounded eminence on the medial wall of the aditus, above and behind the prominence of the facial nerve canal, corresponds to the position of the lateral semicircular canal. Its summit projects in the course of the fenestra vestibuli and is pierced by a small aperture that transits the tendon of stapedius. The cavity within the pyramidal eminence is prolonged down and again in front of the facial nerve canal; it communicates with the canal by an aperture by way of which a small branch of the facial nerve passes to stapedius. The fossa incudis is a small despair within the decrease and posterior a half of the epitympanic recess. It accommodates the quick means of the incus, which is fixed to the fossa by ligamentous fibres. All of those extensions of the mastoid air cells are pathologically important since an infection could spread to the buildings round them. Mastoiditis Mastoid antrum the mastoid antrum is an air sinus within the petrous a half of the temporal bone. The aditus to the mastoid antrum, which leads again from the epitympanic recess, opens within the upper a part of its anterior wall. The sigmoid sinus lies some distance posteriorly; the space can be extremely variable and relies on the degree of pneumatization of the mastoid. The roof is fashioned by the tegmen tympani, and so the antrum lies under the middle cranial fossa and the temporal lobe of the brain. The lateral wall, which offers the usual surgical strategy to the cavity, is shaped by the postmeatal strategy of the squamous a part of the temporal bone. This is simply 2 mm thick at birth but increases at a mean rate of 1 mm a year, attaining a final thickness of 12�15 mm. The superior facet of the triangle, the supramastoid crest, is stage with the floor of the center cranial fossa; the anteroinferior facet, which varieties the posterosuperior margin of the exterior acoustic meatus, indicates approximately the place of the descending part of the facial nerve canal; and the posterior side, shaped by a posterior vertical tangent to the posterior margin of the external acoustic meatus, is anterior to the sigmoid sinus. The grownup capacity of the mastoid antrum is variable, but on average is 1 ml, with a general diameter of 10 mm.