Lucipro
Lucipro dosages: 1000 mg, 750 mg, 500 mg, 250 mg
Lucipro packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Generic 500 mg lucipro otc
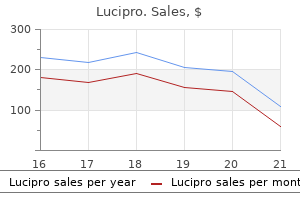
These mutations are in multiple genes within the colorectal epithelium and make it vulnerable to rapid and multifocal carcinogenesis first line antibiotics for acne 750 mg lucipro cheap with amex. Clinically the syndrome presents as dominant inheritance of a quantity of colorectal adenomas and younger age of onset carcinomas virus 7g7 buy generic lucipro 250 mg line. These polyps embody adenomas, serrated polyps and, characteristically, hamartomas. There are typically relatively few synchronous lesions (typically lower than 20) but cumulative totals can grow. The first household reported was of Ashkenazi Jewish heritage, a typical factor amongst reported cases. Colonoscopy with polypectomy could suffice, but if cancer is identified, then an extended resection should be thought of. The pathognomonic signs are macrocepahaly and multiple cutaneous trichilemmomas and papillomas. These embody fibromas, lipomas, neuromas, ganglioneuromas, neurofibromas, adenomas, serrated polyps and juvenile-like hamartomas. Twenty-four had upper gastrointestinal and colorectal polyps, and nine (13%) had colorectal cancer. Physical exam beginning at 18 years of age or 5 years earlier than the earliest cancer was identified within the household. Monthly breast self-examinations and an annual scientific examination starting at 18 years of age. Mammography beginning at 30 years of age, or 5 years younger than the earliest family case of breast cancer; three. Colonoscopy starting at 20 years of age and repeated each 1 to 3 years depending on the findings on the examination. Pelvic ultrasound at 35�40 years of age, or 5 years previous to the earliest household case of endometrial most cancers. In the massive intestine, the juvenile polyps typically develop in childhood and may develop adenomatous dysplasia. The chance of adenomatous dysplasia in the juvenile polyps suggests that common surveillance is indicated. Polyps start to grow within the first 10 years of life and the number varies between 50 and 200. They are sometimes brilliant purple and pedunculated, with polyps rising on the stalks of other polyps. Sporadic instances without a household history could additionally be because of a new mutation or weak penetrance in other relations. Juvenile polyposis of infancy is extraordinarily rare but has an unfavourable prognosis. There could also be increased susceptibility to pneumonia, probably because of the malnutrition and general debility. These manifestations result in anemia, hypoproteinemia, anasarca, failure to thrive and finally dying within two years of life in 90% of infants. They are mainly hamartomas of the lamina propria of the epithelium and feature dilated cystic glands with tall columnar epithelium and an expanded lamina propria with an inflammatory infiltrate consisting of neutrophils, eosinophils and a few lymphocytes. Sometimes a polyp or the rectum itself might prolapse, or there might be belly ache and diarrhoea. Laboratory findings could embody anaemia, hypoproteinaemia, hypokalaemia and pores and skin check anergy. If no mutation is discovered, first-degree relatives should be screened starting on the age of 15. If the first upper and lower endoscopies are negative for polyposis, surveillance could be performed in one to two years. With consistently negative examination the screening interval may be steadily prolonged to each three years. If juvenile polyps are found, therapy is decided by the variety of polyps and the flexibility to control them endoscopically. For kids with generalised juvenile polyposis and hypoproteinaemia, failure to thrive or situations of intussusception, surgical procedure is beneficial. Other troublesome signs, similar to bleeding and diarrhoea, may also be a sign for surgical procedure. Patients with any suspicion of dysplasia or most cancers are suggested to have an operation. Because of the excessive risk of colorectal cancer, most authors imagine that every one polyps, symptomatic or not, must be removed endoscopically or surgically. Colonoscopic polypectomy followed by colonoscopic surveillance is a reasonable various, so long as polyp clearance is possible and affected person compliance is good. Of these, 121 had been colorectal, including 41 partial colectomy, fifty six subtotal or complete colectomy, 7 restorative proctocolectomy, 3 total proctocolectomy with ileostomy, 2 abdomino-perineal resection and 12 operative polypectomy. The remaining 17 operations concerned the abdomen in 12 cases, and the small bowel in 5 circumstances. Almost half (47%) of the latter contained foci of epithelial, whereas only 9% of typical juvenile polyps were dysplastic. The household can then be triaged into affected and Management 857 need for lifetime surveillance of any remaining colon. In many patients, particularly these coming to surgical procedure, the tendency to type polyps varies but could be extreme. Factors contributing to the choice embrace symptoms, phenotype, age, co-morbidities, extent of cancer if present, sphincter perform and surgical experience. Gastric polyps are tougher to handle endoscopically than colorectal polyps, because the gastric lesions tend to be diffuse. Patients so affected usually have severe anemia and can eventually require gastrectomy. In patients with significant duodenal or small bowel polyps, polypectomy ought to be performed either endoscopically before surgical procedure or at the time of surgical procedure. After surgery, surveillance of residual components of the gastrointestinal tract should be resumed. This risk of most cancers was first appreciated within the unique family described by Peutz. The age of demise in affected members of the family was considerably younger (38 years) when compared to that in unaffected members (69 years) and was often as a outcome of intestinal obstruction and cancer. Non-digestive organs at risk for most cancers embrace breast (54%), ovary (21%), lung (15%) and uterus (9%). The lips and perioral region (94%), arms (74%) and ft (62%) are mostly affected. Peutz�Jeghers polyps are hamartomas, recognized by the distinctive muscularis mucosae operating in all through the polyp epithelium.
Generic 250 mg lucipro amex
An Alternative to Total Abdominal Colectomy for the Treatment of Severe antibiotics for uti in rabbits lucipro 500 mg on-line, Complicated Clostridium difficile Associated Disease antibiotics for sinusitis lucipro 500 mg order overnight delivery. Mucosaassociated bacterial density in relation to human terminal ileum and colonic biopsy samples. Empiric antibiotic choice strategies for healthcareassociated pneumonia, intra-abdominal infections, and catheter-associated bacteremia. Quantitative determinants of the antibody response to the capsular polysaccharide of Bacteroides fragilis in an animal model of intra-abdominal abscess formation. Sepsis, systemic inflammatory response, and a number of organ dysfunction syndrome: the mystery continues. Identification of sufferers in danger for development of tertiary peritonitis on a surgical intensive care unit. Biomarkers (Procalcitonin, C Reactive Protein, anctate) as Predictors of Mortality in Surgical Patients with Complicated Intra-Abdominal Infection. Magnetic resonance imaging of acute appendicitis in pregnancy: A 5-year multiinstitutional examine. A technique for estimating the risk of surgical website an infection in patients with abdominal colorectal procedures. The Mannheim peritonitis index: An instrument for the intraoperative prognosis of peritonitis. Comparative research of left colonic Peritonitis Severity Score and Mannheim Peritonitis Index. Clinical comparison of antibiotic mixture within the remedy of peritonitis and associated combined aerobic and anaerobic surgical sepsis. Clinical and scientific significance of source control in abdominal infections: Summary of a symposium. Nonsurgical remedy of appendiceal abscess or phlegmon: A systematic review and meta-analysis. Comparison of endoscopic closure modalities for standardized colonic perforations in a porcine colon model. Severe disease on endoscopy and steroid use increase the chance for bowel perforation throughout colonoscopy in inflammatory bowel disease patients. Pressurized pulse irrigation with saline reduces surgical-site infections following main hepatobiliary and pancreatic surgery: Randomized managed trial. Surgical wound irrigation: A call for evidence-based standardization of scientific follow. Reducing the danger of surgical site infections: Does chlorhexidine gluconate present a risk reduction benefit Intraperitoneal irrigation with povidone iodine solution for prevention of intra-abdominal abscesses in the bacterially contaminated abdomen. Direct peritoneal resuscitation accelerates primary abdominal wall closure after injury management surgical procedure. Adjunctive remedy of belly catastrophes and sepsis with direct peritoneal resuscitation: Indications for use in acute care surgical procedure. Perioperative normothermia to scale back the incidence of surgical wound an infection and shorten hospitalization. Acute hyperglycemia and the innate immune system: Clinical, cellular, and molecular features. Surviving sepsis marketing campaign: International pointers for administration of extreme sepsis and septic shock; 2012. Economic consequences of failure of preliminary antibiotic therapy in hospitalized adults with difficult intraabdominal infections. The Surgical Infection Society revised guideline on the management of intra-abdominal an infection. Antibiotic kinetics within the febrile multiple-system trauma affected person in important care. Antibiotic prophylaxis to scale back respiratory tract infections and mortality in adults receiving intensive care. The international sepsis forum consensus convention on definitions of infection within the intensive care unit. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: A multicentre, parallel-group, randomised, open-label trial. Active Negative Pressure Peritoneal Therapy After Abbreviated Laparotomy: the Intraperitoneal Vacuum Randomized Controlled Trial. Supplemental perioperative oxygen and the danger of surgical wound an infection: A randomized controlled trial. Importance of perioperative glycemic control generally surgery: A report from the Surgical Care and Outcomes Assessment Program. The effects of steroids during sepsis rely upon dose and severity of sickness: An updated meta-analysis. Treatment of gram-negative bacteremia and shock with human antiserum to a mutant Escherichia coli. Human recombinant protein C for severe sepsis and septic shock in adult and paediatric patients. Extracorporeal endotoxin removal for the treatment of sepsis: Endotoxin adsorption cartridge (Toraymyxin). The presence of colonic dilatation within the setting of acute severe colitis is termed toxic colitis or toxic megacolon (transverse colon diameter >6 cm). Severe acute colitis was outlined as passage of a minimal of six bloody stools every day, pulse fee of a minimal of 90 beats per minute, temperature of at least 37. Severe diarrhoea might lead to a level of hypovolaemia with associated hypotension and tachycardia. Due to insensible fluid losses and 1422 anorexia, weight loss with a fall in serum albumin is often present. Many patients may have a fever, secondary to translocation of micro organism throughout the infected colonic wall, causing a systemic inflammatory response. The normal haustral sample is absent within the concerned segments, and pseudopolyps typically lengthen into the lumen. Radiographic proof of mucosal islands inside forty eight hours of presentation has been shown to be predictive of want for colectomy. A finding of tenderness and guarding in the right iliac fossa is a cause for concern, as it may point out imminent perforation of a distended caecum, the portion of the colonic wall which is the thinnest. On presentation, laboratory investigations sometimes reveal an anaemia, secondary to blood loss within the stools. Computed tomography of the stomach and pelvis, although not obligatory, will typically assist within the prognosis of acute colitis. This suggests that encountering environmental antigens at an early age might facilitate maturation of the mucosal immune system, which proves protecting. The host microbiome carries out a range of helpful functions in people, including digesting substrates inaccessible to host enzymes, educating the immune system and repressing the expansion of disease inflicting organisms. The patient had a localised perforation of the transverse colon at emergency laparoscopic complete colectomy. This could be performed via the normal open strategy, or laterally by way of minimally invasive methods.
Syndromes
- Nonsteroidal anti-inflammatory drugs (NSAIDS)
- Nausea
- For females, place the bag over the labia.
- Skin creams containing capsaicin
- A thin, insulated wire called a lead, or electrode that is placed into the brain
- Delayed closure of fontanelles ("soft spots")
- MCV greater than upper limit of normal: macrocytic anemia
Lucipro 250 mg buy lowest price
This article will explore the totally different aetiologies infection hair follicle order lucipro 250 mg without a prescription, diagnostic modalities and management of acute mesenteric ischaemia antimicrobial pillows 1000 mg lucipro buy with mastercard. However, it is important to recognise that small intestinal mesenteric ischaemia also can involve the colon, particularly the proper facet. The mesenteric vasculature can be extremely variable, though there are specific constants that allow practitioners to formulate a analysis and administration strategies. The coeliac artery primarily supplies the foregut from the distal oesophagus to the duodenum. The distal rectum is provided by branches of the internal iliac (hypogastric) arteries by way of the center and inferior rectal (haemorrhoidal) arteries. The coeliac artery branches from the aorta slightly below the diaphragmatic hiatus, sometimes at the level of the T12 vertebral physique. It arises nearly perpendicularly to the aorta, and it instantly offers off three branches: the left gastric artery, the common hepatic artery and the splenic artery. Together, these branches provide blood to the distal oesophagus, stomach, liver, gall bladder, duodenum, pancreas and spleen. There is extensive collateralisation amongst these branches, which helps shield the stomach from ischaemia. The widespread hepatic artery gives off the best gastric artery, which meets the left gastric artery alongside the lesser curve of the stomach. The splenic artery gives off the left gastroepiploic artery, which meets the right gastroepiploic artery (a branch of the hepatic artery) along the higher curve of the abdomen. The liver receives approximately 60% to 70% of its blood provide from the portal vein, making the hepatic artery a minor contributor. This twin blood provide also protects the liver from ischaemia throughout insults to the mesenteric vasculature. The gall bladder receives blood via the cystic artery (usually as a branch of the right hepatic artery). It then runs inferiorly, coursing initially posterior to the body of the pancreas. The first of these branches is the inferior pancreaticoduodenal artery, as described above, adopted by the middle colic artery, which provides the transverse colon. The center colic artery typically divides into a right department and left branch, such that the best branch will provide the proximal transverse colon and the left department will supply the distal transverse colon. This community of arcades forms the marginal artery of Dwight, which runs parallel to the small intestine and permits for communication amongst the jejunal and ileal branches. The left colic artery then branches into an ascending limb and a descending limb, which are parts of the marginal artery of Drummond. The ascending limb communicates immediately with the left branch of the center colic artery and the descending limb travels distally to provide the left colon. This vessel runs near the foundation of the mesentery and provides an arterio-arterial connection between the proximal portions of each vessels. The inside iliac (hypogastric) arteries provide blood to the center and distal rectum by way of two paired arteries: the center and inferior rectal (haemorrhoidal) arteries. These branches arise from the inner pudendal arteries, which are in flip branches of the interior iliac arteries. Terminal arterial branches arise from the marginal arteries and arcades to provide blood directly to the intestinal wall. Under the serosa, these arteries then divide into numerous smaller branches and kind a community that in the end anastomose on the antimesenteric aspect of the gut. These branches penetrate the muscularis propria and type another network of vessels. Ultimately, the arterioles attain the mucosal layer and once more form a community of vessels. The venous drainage of the intestine mirrors the arterial routes, with a couple of exceptions. The inferior mesenteric vein runs within the retroperitoneum to mix with the splenic vein or superior mesenteric vein. The superior mesenteric vein and the splenic vein join at the portal confluence to kind the portal vein, which then enters the liver. The gastrocolic trunk of Henle is a crucial construction made up of a confluence of the proper colic, proper gastroepiploic and anterio-superior pancreaticoduodenal vein. The embolus is usually a dislodged thrombus, and underlying aetiologies embody atrial fibrillation, myocardial infarction with wall motion abnormalities, infective endocarditis, valvular disease or aortic aneurysm. An embolus at this location ends in ischaemia from the distal jejunum to the ascending colon with relative sparing of the duodenum, proximal jejunum and transverse colon. There are often few collateral vessels to compensate for the sudden and dramatic lower in blood flow, which places these sufferers at excessive risk of morbidity and mortality. Patients with acute embolic ischaemia sometimes experience a sudden onset of severe stomach pain. It can additionally be important to consider for synchronous embolisms, including to the mind and extremities, as approximately 15% to 20% of embolic mesenteric ischaemia cases will have a quantity of embolisms. In the setting of peritonitis, diagnostic confirmation is usually made in the working room. In the absence of peritoneal signs or within the setting of an equivocal historical past and physical, the analysis is made with imaging research. Computed tomography has turn out to be the check of choice for the evaluation of mesenteric ischaemia due to its broad availability, rapidity and accuracy. Laboratory research often present a marked leucocytosis with a left shift, lactic acidosis and increased base deficit. Management includes haemodynamic resuscitation with operative revascularisation and resection of non-viable gut. Patients with a thrombotic occasion will usually have a history of continual ischaemia and underlying mesenteric atherosclerosis. The atherosclerosis develops over time and finally a important stage of stenosis accumulates. During a period of relative low move to the mesenteric vessel, this critical lesion thromboses. Therefore, thrombosis usually affects a larger portion of the intestine, from the duodenum to the transverse colon. Arterial thrombosis seems to have the best mortality of all of the causes of mesenteric ischaemia, roughly 77% after surgical administration. This poor outcome is probably associated to the need for prolonged bowel resection due to more in depth bowel ischaemia and infarction. Previous persistent signs might include concern of eating, weight loss or post-prandial belly ache. The bodily exam amongst those with thrombotic mesenteric ischaemia is much like these with an embolic occasion: pain out of proportion to the exam. The therapy of arterial thrombosis causing mesenteric ischaemia is much like that of arterial embolism. Venous Mesenteric Ischaemia Venous thrombosis is the least common explanation for mesenteric ischaemia and accounts for approximately 5% to 10% of instances. Mesenteric venous thrombosis typically happens within the setting of a systemic dysfunction.
Lucipro 250 mg safe
Similarly antibiotic guide pdf buy lucipro 250 mg otc, if a mucous fistula has been created within the proximal small bowel antimicrobial zone of inhibition discount lucipro 1000 mg without a prescription, for instance for the administration of an anastomotic leak following bariatric surgery, then entry to this section of bowel could allow successful enteral feeding by way of a radiologically-placed feeding tube. The feeding tube can be secured within a stoma appliance, using a waterproof seal and plastic cone to perforate the appliance on the site of the fistula, thus permitting feed to be administered through the distal portion of the fistula whilst effluent drains through the proximal portion concurrently. The amount of nitrogen needed (usually expressed as grams of nitrogen per kg physique weight or relative to kcal energy supplied) increases with the degree of metabolic stress, from 0. In sepsis and different crucial sickness states, the metabolism of nitrogen is directed in direction of synthesis of acute part proteins, and pathologically exaggerated conversion of amino acids to glucose (gluconeogenesis). Protein catabolism due to this fact persists in sepsis, despite apparently adequate provision of energy. It is due to this fact important to deal with sepsis before provision of nutrition may be expected to lead to restoration of nitrogen steadiness. There is often little to be gained by administration of greater than 14 g of nitrogen per day and obvious failure to restore lean body mass on this setting should immediate a vigorous seek for inadequately handled infection (see above). Vitamins, Trace Elements and Minerals the availability of nutritional vitamins, trace elements and minerals is an essential component of all parenteral regimens. Most sufferers who require parenteral vitamin will have had pre-existing illness and should already be poor in these necessary dietary constituents. Lipid malabsorption may lead to deficiencies of the fat-soluble nutritional vitamins A, D, E and K. Water-soluble nutritional vitamins B and C are necessary coenzymes in energy manufacturing, collagen formation and wound therapeutic. Vitamin C requirements may rise sharply to as a lot as 80 mg per day throughout stress or after surgery. The consumption of vitamins C and E can also rise as a consequence of their role as free radical scavengers in situations such as sepsis and important illness. Magnesium concentrations could fall quickly in sufferers with excessive output stomas or diarrhoea, and the inflammatory response might result in alterations of iron and zinc metabolism, which lead to decreased availability for haemopoiesis, Acute Intestinal Failure 1463 eighty one. By definition, a excessive output intestinal fistula produces more than 500 mL of effluent each day. When the fistula or stoma output seems extreme (particularly when it has beforehand been stable), a cautious seek for an underlying trigger should be made. Most sufferers with a stoma or fistula output persistently in extra of 1 L, even with normal oral consumption, would require interventions designed to scale back fistula or stoma effluent and curtail fluid and electrolyte losses. Accurate fluid balance is important, with regular weighing and monitoring of serum urea and electrolyte concentrations, often every day till day by day necessities may be estimated, provided and stability is achieved. Measurement of urinary sodium focus is commonly of value in this setting, notably if renal function is regular, and may help to distinguish the hyponatraemia related to adequate sodium status however extreme water administration from the hyponatraemia of sodium depletion. Urinary sodium concentrations of lower than 20 mmol/L are, nevertheless, often indicative of the latter. Intestinal losses of magnesium could be significant, particularly in stomas or fistulas affecting the very proximal small gut. Significant or persistent hypomagnesaemia (which can lead to tetany), is finest handled by slow intravenous replacement. High-output stomas and fistulas could reply to alteration of fluid intake and a cautious assessment of the quantity and kind of fluid being consumed is important, particularly if the output appears extreme for the quantity of small intestine in continuity. The fluid within the proximal small gut is otonic, because the intercellular junctions within the jeunum are extremely permeable, turning into tighter in the distal ileum and tighter still within the colon. The proximal bowel is due to this fact unable to preserve a concentration gradient and water freely equilibrates throughout the jejunal barrier by osmosis. Effluent from stomas or fistulas proximal to the distal ileum is therefore isotonic 81 1464 Chapter 81 Intestinal Failure and consumption of oral hypo-osmolar fluids similar to water and delicate drinks (especially these with sugar or artificial sweeteners) might considerably increase stoma or fistula output. This could be prevented by restriction of oral intake to 1,000 to 1,500 mL per day, and educating the patient that thirst in a setting of a high output stoma or fistula is finest treated, counter intuitively, by limiting oral consumption and growing intravenous fluids instead. Replacement of oral hypo-osmolar fluids with electrolyte options reduces sodium losses and may cut back stoma and fistula flux. In addition, inhibition of other gut hormones could resulted in negative effects including precipitation of diabetes and pancreatic exocrine insufficiency and liver dysfunction. Improvement in bodily properly being associated with management of sepsis and reversal of nutritional impairment is gradual and may take many months. Psychological difficulties are regularly encountered at this stage of restoration and should also be addressed. Stomas and wound problems could result in vital nervousness with respect to body image, particularly in younger sufferers. Almost all sufferers profit from an honest and sympathetic dialogue about their condition and its prognosis, and recognize active involvement in agreeing and carrying out the required treatment plan. The probably timescale for improvement and reconstructive surgical procedure (where this is needed) must be defined. In sufferers with open stomach wounds, a period of six months is often required earlier than the wound has granulated and the method of neoperitonealisation has taken place sufficiently for reconstructive surgery to be undertaken. This might require training the affected person or a family member in strategies for line care and administration of parenteral nutrition at Medical Therapy Pharmacological manipulation of stoma or fistula output may be of profit when mixed with restriction of oral intake. Regular oral Loperamide is often effective in doses of eight to 32 mg per day and codeine phosphate (60 mg four times daily) may be equally useful. Initially, quick bowel syndrome associated with huge small intestinal resection or proximal fistulation appears to be associated with gastric hypersecretion, because of the lack of the unfavorable suggestions from the small bowel on gastric acid secretion on account of absence of hormones, corresponding to gastrin inhibitory polypeptide, which occurs following resection (or exclusion) of small intestine and its enteroendocrine cells. It is unclear whether the ensuing hypergastrinaemia and increased gastric acid and fluid secretion, which occurs in animal fashions of short bowel syndrome, truly happens in man,eighty two and animal studies have instructed that the response may only final for as a lot as three to six months. Nevertheless, clinical studies in patients with quick bowel syndrome and high-output stomas have proven that proton pump inhibitors do cut back stoma effluent. The use of somatostatin analogues such as Octreotide for the administration of high-output stomas and fistulas is controversial. These agents work by inhibiting gastric, pancreatic and biliary secretion, and decreasing intestinal blood flow and motility. Once the affected person is stable, sepsis has been treated and efficient wound and/or fistula administration put in place, a fistulogram and distal contrast research could also be of profit in delineating fistula anatomy, with the precise purpose of establishing whether spontaneous closure is probably going (see below). This is most likely going not solely to be of worth in planning surgery but may be of prognostic importance (for instance, by exhibiting the quantity of residual small intestine obtainable for restoration of continuity). The intestinal tract distal to a fistula ought to never be assumed to be wholesome, even in patients without intrinsic intestinal disease, as a result of vital strictures because of unrecognised bowel harm or ischaemia during the management of abdominal sepsis can be simply ignored, leading to post-operative intestinal obstruction and/or anastomotic leakage after reconstructive surgical procedure. Contrast studies of the proximal and distal gastrointestinal tracts and fistulography are routinely undertaken, and, the place applicable, imaging of the biliary and urogenital tracts can also be required. In all sufferers with an abdominal wall defect, cross-sectional imaging is of importance to be able to delineate the scale and form of the defect in the belly wall fascia which must be reconstructed. The elements, which decide the probability of spontaneous fistula healing, are proven in Table 81. Similarly, the function of somatostatin and its analogues in selling the therapeutic of intestinal fistulas stays controversial and unproven. Although meta-analyses of the role of somatostatin analogues have instructed that the rate of fistula therapeutic could additionally be increased,86 these studies have virtually invariably included pancreatic fistulas as properly as enterocutaneous fistulas. An ongoing Cochrane evaluate has been established to determine whether or not Somatostatin analogues promote healing in specifically enterocutaneous fistulas,87 however it appears unlikely that a fistula whose anatomy precludes spontaneous healing could possibly be induced to heal by simply reducing the amount of effluent passing via it.
Cheap 1000 mg lucipro visa
A right higher quadrant port should be positioned to facilitate acceptable triangulation antibiotics starting with z 750 mg lucipro generic mastercard. Many occasions a left decrease quadrant port is used to aid left colon and splenic flexure mobilisation antibiotics for acne bad for you 1000 mg lucipro order free shipping. Once pneumoperitoneum is achieved and ports are placed, the rectosigmoid is retracted medially and the peritoneum is incised on the white line of Toldt. This lateral peritoneal incision is then taken to the level of the splenic flexure. Lateral-to-medial dissection should be continued till the ureter is recognized and the upper rectum is dissected. If the process is to be completed intracorporeally, the sigmoid colon is then retracted anteriorly and the peritoneum is incised on the right side of the colon from the sacral promontory to the ligament of Treitz. The inferior mesenteric vascular pedicle is identified and is split with either a vascular staple load or a vessel-sealing device. The dissection plane is recognized and the peritoneum is scored alongside that plane from the sacral promontory to the inferior mesenteric vascular pedicle. Once the ureter is clearly identified and traced, the vascular pedicle is dissected out and divided either between clips, with a stapler or an vitality device. The medial-to-lateral dissection is then continued to the posterolateral edge of the descending colon, sigmoid colon and increasing down into the pelvis. The rectosigmoid is retracted medially and the lateral peritoneal attachments are released using electrocautery or a 52 Laparoscopic Sigmoid colectomy Patient positioning � low lithotomy, rolled proper, Trendelenburg, arms tucked surgeon position � right of patient Monitor Monitor Assistant 5 mm working port 12 mm camera port (optional extraction site) Assistant (2nd option) Optional 5 mm port to mobilise splenic flexure and pelvic dissection Surgeon Monitor 5 mm or 12 mm port Hand-port website (pfannenstiel incision) Steele 52. Based on the length and mobility of the remainder of the descending colon, a decision ought to be made concerning the necessity of splenic flexure mobilisation. If additional size is required to facilitate a tension-free anastomosis, the splenic flexure must be taken down. Omental attachments to the anterior transverse colon are also divided at least to the extent of the mid-transverse colon. The deliberate proximal transection level is grasped and introduced into the pelvis to affirm sufficient size. If additional size is needed, it could be essential to carry out a better division of the inferior mesenteric vein. In this method, we start with a affected person within the reverse Trendelenburg position with the left aspect elevated. Dividing the attachments proper above the pancreatic tail will allow entry to the lesser sac. The patient is then placed in a head down place, and the sacral promontory is identified. With either strategy, the colon is then divided at the proximal transection level using either a linear stapling gadget or by sharp division after clamping the colon with a laparoscopic bulldog Glassman clamp. The distal transection is similarly carried out on the degree of the proximal rectum at the sacral promontory using a linear laparoscopic stapler. Transanal removal could also be carried out by putting the specimen in an endoscopic retrieval bag and bringing the bag out by way of the opened rectal stump (sharp distal transection is preferred over stapled if this is the meant method of extraction). Alternatively, the specimen could also be eliminated through a small Pfannenstiel incision or by way of an extended decrease abdominal port-site incision, usually with the use of a wound protector. Similar to an open process, the proximal bowel could additionally be extra-corporealised and the anvil secured into place utilizing a purse-string suture. The proximal colon is then positioned back into the stomach and the port is closed either temporarily with sutures on Rumel tourniquets or by closing off the wound protector with the help of a clamp. The anvil is then grasped with an anvil grasper positioned via a 12-mm port, and the anvil with its connected proximal colon is brought into the pelvis. This is done carefully so as to guarantee no twisting of the colon, which inherently compromises the blood provide. Meanwhile, the assistant serially dilates the anus earlier than inserting the top of the circular stapler. If any question remains relating to the constancy of the anastomosis, a diverting loop ileostomy ought to be performed. Overall, the technical features are similar to both the open and straight laparoscopic approaches. We use the Hasson method for stomach entry and institution of pneumoperitoneum. A 5-mm epigastric port should be positioned to facilitate appropriate triangulation. The colon mobilisation might then be performed utilizing both the lateral-to-medial or medial-to-lateral method as beforehand described. The splenic flexure mobilisation is much like an open approach, with the non-dominant and dominant hand alternating relying on ease of dissection (see Video 52. The proximal transection level is identified and the colon is divided with a linear stapler or between clamps. The proximal rectum is then divided using a linear stapler and the specimen is eliminated. As with prior approaches, the process is accomplished by securing the anvil on the finish of the proximal colon with a purse-string suture of 2-0 prolene suture. An assistant then serially dilates the anus and inserts the top of the circular stapler. Whilst maintaining fixed communication with the surgeon, the assistant brings the point of the stapler head out of the rectal stump adjoining to the staple line. Following the stapled anastomosis, proceed with a proctoscopic examination and air-leak check. Likely for the latter reason, the robot is being utilised for numerous colorectal applications, each with its specific cart and port placement. The purpose of this section is to familiarise the surgeon with the technical elements of port placement, cart placement and surgical steps of robotic-assisted sigmoid colectomy quite than to act as an all-encompassing dialogue together with the fundamental capabilities of the robotic. It must also be noted that cart and port positioning will probably change as totally different robotic platforms are developed. It is preferable to decide previous to the beginning of the case whether a single or a number of cart positions shall be used. The capability to achieve an sufficient dissection from a single robot position depends on a variety of elements, with the principal ones being correct port and cart placement, affected person physique habitus and stage of the illness. Utilise a left lateral docking station for normal sigmoid colectomy, and place a laparoscopic-assist port in case proximal dissection is required. The bedside assistant should also be cognizant of sudden, speedy actions of the robotic arms during dissection, which may lead to an unintentional assault of the arms, head and torso of the unsuspecting assistant. The arms are tucked at the sides, and the patient is secured to the table at the chest degree with tape. Pressure points are padded, with special consideration paid to the best facet, as the affected person will spend nearly all of the process in the Trendelenburg position with the left facet elevated. Unlike traditional laparoscopy, this can be achieved approximately one to two finger widths superior and proper of the umbilicus followed by the placement of a normal 12-mm laparoscopic trocar in the same location.
1000 mg lucipro order mastercard
The trigger may be dilatation throughout surgical procedure or denervation since the inside sphincter receives most of its nerve enter from the lower part of the circular rectal musculature infection nursing interventions 250 mg lucipro order otc. Physiological testing can assess proprioception in the pouch by measuring the volume wanted to elicit the primary feeling of pouch filling homemade antibiotics for acne lucipro 250 mg buy generic on-line, the brink for urge and most tolerated volumes. Pouch motility could also be disturbed and sensory parameters impaired within the dilated pouch above a stricture or retained segment of rectum. Endoanal ultrasound, if tolerated within the unanaesthetised patient, will provide dependable anatomical assessment of the sphincters that may complement the evaluation done by the examining finger and manometry. At instances, examination underneath anesthesia, particularly in sufferers affected by surgical complications where pain is a serious concern, is informative. This is finest achieved in high-volume establishments amongst skilled surgical teams. It is an operation meant to provide the absolute best bowel perform for the person affected person whose remaining life span is often around 50 years. However, even in one of the best hands, restorative proctocolectomy is an operation that also carries a complication price of no much less than 30%. During the operation, there must be a tensionfree anastomosis, which entails a full mobilisation of the small bowel mesentery with mesenteric lengthening procedures that could be very delicate. Achieving an anastomosis within 1 to 2 cm distance from the dentate line is crucial. This is a specific downside in males and also in the laparoscopic setting with a scarcity of good cross-stapling instruments to be used deep in the pelvis. When and tips on how to finest assemble a overlaying loop ileostomy is one other crucial problem. Marks pouchitis triad and histopathologic index (defined by 6 stools/day from baseline; 4 factors for oedema, granularity, friability, lack of vascular sample or ulceration; 4 points for polymorphonuclear leucocyte infiltration and percent of ulceration per low-power field). The main distinction is the inclusion of persistent irritation throughout the variables of the histological standards (see Table sixty eight. It happens in about one-third of patients inside one year after surgery, and after 10 years, 50% of topics may have had no much less than one episode of pouchitis. Calprotectin and lactoferrin are proteins derived from neutrophils and may be measured in stool throughout intestinal inflammation. Defaecography and anorectal manometry can be used to assess useful problems, which may not present with pouchitis like symptoms, corresponding to in emptying difficulties. The ileal mucosa of the pouch undergoes histopathological modifications, which embrace: villous atrophy, crypt hyperplasia and the appearance of goblet cells. A large pouch might empty ineffectively, thereby rising the faecal stasis and the risk of pouchitis. Bile acid malabsorption would possibly trigger bile irritation of the pouch mucosa and diarrhoea, during which case bile-acid�binding brokers such as cholestyramine could be thought to be effective, but actually that is hardly ever useful. The incidence of bacterial overgrowth may enhance bowel frequency with watery stools and trigger stomach cramps. It has been advised that a lowcarbohydrate, low-fibre and high-protein diet could also be therapeutic. Metronidazole (15 to 20 mg/kg/day) or ciprofloxacin (500 mg twice daily) for 14 days are essentially the most generally used. However, there are just a few small randomised trials for both metronidazole and ciprofloxacin, both of which fared higher than placebo. Ciprofloxacin was more effective in inducing a remission and had less side effects compared to metronidazole. Eighty-two % of the sufferers had been in concomitant treatment with immunomodulatory agents. After a median follow-up time of 20 months, 56% and 43% of sufferers, respectively, maintained a sustained response. Complete (defined as cessation of diarrhoea and urgency) and partial (defined as improvement of symptoms) response have been assessed at weeks 8, 26 and fifty two: respectively, 21%, 33% and 27% of patients achieved a complete response at weeks 8, 26 and fifty two, while 63%, 33% and 18% achieved partial response on the similar time factors. Forty % of sufferers stopped remedy (31% had been main non-responders, 31% for a poor response, 38% for adverse events). Another less complicated different that has been instructed is to take away the bevelled plastic protector from the thin fork of the stapling system, allowing the staple line to be accomplished to the tip of the stapled efferent limb of the J pouch. In everlasting 1296 Chapter 68 Pouch Dysfunction in Colitis torsion, the ache turns into fixed and there are systemic signs from the process of strangulation. The blind afferent limb can even cause useful problems as a outcome of faecal retention and poor pouch emptying associated with pouchitis. Torsion of the afferent limb may be secondary to obstruction due to an acute angulation of the inlet bowel at this point or may be related to prolapse or intussusceptions of the afferent limb on the junction with the pouch. The prognosis is made on symptoms of obstruction, and confirmation is made in contrast enema. To avoid this drawback, light finger dilatation by palpation of the anastomosis when the affected person is discharged from hospital, and at four weeks post-operatively is suggested. Patients might present with stricture once they come again for loop ileostomy closure. This may be dilated during anaesthesia at loop ileostomy closure, but if the stricture is tight, dilation often has to be repeated. The other more problematic state of affairs are the strictures seen after anastomotic leaks and pelvic sepsis since they embrace much more scar tissues. The perfect case for surgical correction is after a stapled anastomosis the place the fibrosis is situated on the prime of the anal canal or in the lower pelvis. In this situation, an entire dissection of the pouch as far as one can reach from the stomach method adopted by an endoanal mucosectomy together with the anastomosis with its surrounding fibrosis is often possible. After the fibrosis is resected, the pouch is delivered via the pelvis and perineum and secured with a hand-sewn endoanal anastomosis. The presenting symptoms are often pelvic pain, basic malaise and profound weight reduction, usually with compromise of pouch perform. If pus is seen during endoscopy, one ought to attempt to localise the anastomotic or pouch defect, which is often located posteriorly. An anastomotic defect can sometimes be visualised with a two-blade anal retractor. One possibility is to incorporate the sinus into the lumen of the pouch by opening the sinus using a linear endocutter. Other strategies embody the insertion of a papillotome or other technique of electrocauthery, however the literature is scarce on the strategies or the results of this. The risk of osteomyelitis of the sacrum ought to at all times be kept in mind for which prolonged therapy with antibiotics even after symptom decision is often beneficial. The Small Pouch Some sufferers might have a very small pouch, which can give rise to functional issues, significantly high bowel frequency and urgency. However, pouch measurement alone might be Surgical Causes of Pouch Dysfunction 1297 solely an explanation for about 20% of all surgical causes of pouch dysfunction. A standard J pouch made of two � 15 cm of terminal ileum will obtain a matured last quantity of 200 to 350 mL six months to one yr post-operatively. However, the vary of measured pouch volumes can be appreciable, various from 65 to 440 mL. The pouch has to be mobilised from the pelvis in order that one other bowel phase can be integrated by a longitudinal antimesenteric incision between the pouch and the augmented bowel.
Smilax Aristolochiifolia (Mexican sarsaparilla) (Sarsaparilla). Lucipro.
- How does Sarsaparilla work?
- Dosing considerations for Sarsaparilla.
- What is Sarsaparilla?
- Are there safety concerns?
- Psoriasis, rheumatoid arthritis, kidney problems, fluid retention, digestive problems, syphilis, gonorrhea, and other conditions.
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96393
Cheap 500 mg lucipro mastercard
We recognise that the worth of a protective stoma stays controversial bacteria fighting drug purchase 1000 mg lucipro otc, however we often perform a protective ileostomy in circumstances with anastomoses decrease than 4�5 cm from the anal verge treatment for dogs fever lucipro 250 mg best. In our experience the morbidity related to fashioning a protective stoma and the problems of stoma closure have been very restricted. There is now good evidence to show that laparoscopic rectal cancer surgery results in better short-term outcomes in comparison with open surgical procedure with none vital distinction in the oncological outcome. Clinicians are increasingly embracing shared decision-making, which is impractical if either the clinician or the affected person lack sufficient data to exercise choice. This is made even more difficult as a outcome of patients come with differing ranges of schooling, information and preconceptions. In distinction, in rectal most cancers the histopathology is modified following the current standard of administration, i. These trials have both used an observation management arm versus a single agent, or remark versus a combination routine, or a single agent versus a mix regimen. Selection of the optimum treatment for the individual in rectal cancer entails difficult choices and stark tradeoffs, and patient desire must be taken into account. Radiation subject size could additionally be tailor-made to the individual affected person, however the radiation dose and the estimated threat of complication relies on population averages. The determination to supply preoperative neoadjuvant therapy is based on outcomes of large groups of patients with various levels, sites and sizes of cancer handled by quite a few totally different surgeons randomised to obtain adjuvant radiation remedy or not. This technique could spare some patients from therapy, which is associated with a spread of acute and long-term unwanted aspect effects, and is unlikely to be efficient. Preoperative radiotherapy with or with out concurrent fluorouracil and leucovorin in T3-T4 rectal cancers: 9. Sphincter preservation following preoperative radiotherapy for rectal most cancers: Report of a randomised trial evaluating short-term radiotherapy vs. Long-term results of a randomised trial evaluating preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal most cancers. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing charges of native recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group Trial 01. Effect of preoperative therapy methods on the result of sufferers with clinical T3, non-metastasized rectal most cancers: A comparison between Dutch and Canadian skilled centers. The Stockholm I trial of preoperative short term radiotherapy in operable rectal carcinoma. Randomised research on preoperative radiotherapy in rectal carcinoma; Stockholm Colorectal Cancer research Group. Short-term preoperative radiotherapy ends in down staging of rectal most cancers: A research of 1316 patients. Neoadjuvant treatment for unresectable rectal most cancers: An interim evaluation of a multicentre randomized research. Consensus statement on the multidisciplinary management of sufferers with recurrent and primary rectal cancer beyond total mesorectal excision planes. Avoiding radical surgery improves early survival in aged patients with rectal most cancers, demonstrating complete medical response after neoadjuvant remedy: Results of a decision-analytic model. Impact of radiotherapy enhance on pathological full response in sufferers with domestically superior rectal most cancers: A systematic evaluate and meta-analysis. Long-term results of a randomized trial in domestically superior rectal most cancers: No benefit from including a brachytherapy enhance. Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal most cancers: A randomised, multicentre, non-inferiority, section three trial. Late adverse effects of radiation remedy for rectal cancer � A systematic overview. Effects of radiation therapy on the construction and function of the pelvic flooring muscle tissue of sufferers with cancer within the pelvic area: A systematic review. Systematic evaluation of radiation therapy toxicity reporting in randomized controlled trials of rectal cancer: A comparison of patient-reported outcomes and clinician toxicity reporting. Effect of preoperative radio(chemo) remedy on long-term useful end result in rectal cancer sufferers: A systematic review and meta-analysis. Capecitabine and oxaliplatin within the preoperative multimodality treatment of rectal cancer: Surgical end factors from National Surgical Adjuvant Breast and Bowel Project trial R-04. Short-course Versus Long-course Preoperative Radiotherapy plus Delayed Surgery within the Treatment of Rectal Cancer: A Meta-analysis. Randomized scientific trial on preoperative radiotherapy 25 Gy in rectal most cancers � Treatment results at 5-year follow-up. Initial outcomes of a randomized controlled trial comparing clinical and pathological downstaging of rectal most cancers after preoperative short-course radiotherapy or long-term chemoradiotherapy, both with delayed surgical procedure. Optimal time interval between neoadjuvant chemoradiotherapy and surgery for rectal most cancers. Patients who endure preoperative chemoradiotherapy for locally advanced rectal most cancers restaged 24. Pre-operative radiotherapy and healing surgical procedure for the management of localized rectal carcinoma. Perineal wound healing after abdominoperineal resection for rectal cancer: A systematic evaluate and metaanalysis. Does Preoperative Radio(chemo)therapy Increase Anastomotic Leakage in Rectal Cancer Surgery Effect of preoperative lengthy course radiotherapy on anastomotic leakage after low anterior resection for rectal most cancers: A meta-analysis. Systematic review of preoperative, intraoperative and postoperative threat factors for colorectal anastomotic leaks. Especially for the elderly and in patients with co-morbidity, rectal resections are major procedures with substantial perioperative morbidity and mortality. Whereas the overall mortality of rectal cancer surgery is 2%�3%, mortality charges in patients over eighty years of age in the range of 10%�15% have been documented in a big inhabitants database, with a six-month mortality as excessive as 15%�25%. Many patients with rectal cancer express an express wish to keep away from a definitive stoma. Very low and intersphincteric anastomoses for distal rectal cancer can avoid a definitive stoma, but the functional outcome is usually poor. The concern in regards to the oncological threat of organ preservation is that some local regrowths is probably not amenable to salvage surgery and that some regrowths could possibly be the source of metastases. In this tradeoff choice process for a person affected person there are broadly two types of concerns. The second sort of issues are more subjective and concern high quality of life issues corresponding to disturbed physique image with a colostomy, impaired anorectal function in distal anastomoses, urogenital dysfunction, and so on. Watch-and-Wait After the pioneering paper by Angelita Habr-Gama from Sao Paulo in 20044 on a watch-and-wait technique for medical full responders, a variety of different constructive reviews have been revealed. There is a large variation in remedy protocols: radiation dose, number of fractions, inclusion of enhance, concomitant chemotherapy mixtures and consolidation chemotherapy. Another important problem in comparing the different series is the proportion of smaller tumours. Whereas the majority of patients in most series are T3 tumours, half of the patients within the prospective research of Appelt et al. In this study, chemoradiation is given with the particular purpose of organ preservation.
Generic lucipro 250 mg with visa
Blunt accidents of the colon are usually seen within the extra mobile sections of the colon including sigmoid colon antibiotic resistance public health purchase lucipro 1000 mg without a prescription, ascending colon and transverse colon antibiotic resistance who 2011 buy lucipro 1000 mg with amex. Devascularisation injuries to the colon also could happen as fast deceleration causes a shearing of the fastened mesenteric peritoneum from a extra cell hollow viscous. Due to the higher threat of delay of analysis as well as the robust affiliation of associated life-threatening accidents to the top and thorax, blunt colonic injuries are Injury Due to Barium Enema Colonic perforation because of barium enema is rare, with an incidence of zero. There is a direct correlation between how much pressure is used in performing the diagnostic check. The damage may be associated to forceful placement of the catheter tip, forceful instillation of barium distinction into the colon or as a end result of extreme inflation of the catheter balloon which causes perforation or laceration of the rectal wall. Individual variations may be required, and nothing should replace correct surgical judgement. Colonoscopic perforation management within the period of laparoscopy: A simple algorithm. Large intramural or retroperitoneal injuries should be drained, Treatment of Rectal Injuries 1369 be evaluated with rigid proctoscopy. An grownup rigid proctoscope is 25 cm in length and the complete surface of the 15 cm grownup rectum should readily be visualised on proctoscopic examination. The diagnostic accuracy of inflexible proctoscopy in diagnosing rectal accidents is 72% to 89% and is dependent upon the location of damage. The sensitivity of inflexible proctoscopy in identifying low or extra-peritoneal rectal accidents was 88% compared to 58% for larger or intra-peritoneal rectal accidents. Grade I injuries are contusions or haematomas of the rectal wall with out evidence of devascularisation, or lacerations of the rectal wall that are partial thickness without evidence of perforation. Intra-peritoneal extravasation requires immediate laparotomy, irrigation and removing of all seen barium. Lavage with urokinase has been reported to be of some benefit in dislodging barium particles. Pre-sacral drainage has fallen from favour when treating penetrating rectal injuries. Besides inflicting affected person discomfort and functioning poorly, the potential for iatrogenic injury during placement of the drain is real. Retrospective research have proven no distinction in the price of pelvic sepsis whether or not pre-sacral drains have been placed. Injuries to the rectum could be divided into two separate classes based on the anatomic location of the harm. Injuries to the rectum above the peritoneal reflection are managed by major repair in the identical method as accidents to the colon. They occur rarely in blunt trauma and, when recognized, are sometimes related to open pelvic fractures and perforation from bone fragments and different life-threatening injuries. Arthurs3 reviewed 28 sufferers undergoing injury control laparotomy for penetrating pelvic accidents. Nearly half had associated extra-peritoneal injuries, main vascular accidents and urologic accidents. Penetrating wounds to the rectum, together with gunshot and stab wounds, could pose a diagnostic challenge. A thorough understanding of the mechanism of damage and a excessive index of suspicion are required to keep away from lacking a doubtlessly life-threatening injury. Digital rectal examination should make particular notice of resting sphincter tone, palpable sphincter defects, mucosal lacerations or the presence of a international body. Overall, digital rectal examination has 33% sensitivity for figuring out rectal injuries. Abnormalities recognized on physical examination should 1370 Chapter 74 Trauma to the Colon, Rectum, Anus and Perineum area, the rectum lacks a serosa and urologic, vascular and reproductive buildings encompass the rectum. Burch studied 100 consecutive sufferers with injuries to the rectum below the peritoneal reflection. All had been handled with colostomy, with a pelvic sepsis rate of 11% and a mortality price of 4%. The authors concluded that faecal diversion was secure and applicable for sufferers with extra-peritoneal rectal accidents. The diploma of tissue destruction and the presence of related accidents are thought to be major determinants of whether or not or not these accidents ought to be diverted. It was concluded that routine diversion and drain placement is pointless for non-destructive extra-peritoneal rectal injuries. The incidence of those occasions is increasing and pose a challenge to the treating doctor or surgeon. Presence of shock, want for transfusion of four units or extra of blood products, diploma of contamination, time from injury, affected person co-morbidities and nature and extent of related injuries ought to all be considered. Shock and transfusion requirement have been associated with anastomotic leakage and septic issues in some research. Conclusion 1371 74 Tear Anal sphincter (torn) (a) (c) Perineal muscle (torn) Perineal muscle (torn) Anal sphincter (b) (d) Anal sphincter (torn) Rectum (torn) 74. Attempts by the patient to retrieve the thing at home could result in additional perianal and intraluminal harm. The objects might cause no symptoms or may be associated with rectal bleeding, discomfort, bowel obstruction or urinary issue. A thorough history and physical examination carried out in a non-judgemental method will allow the attending doctor to determine the character of the international object, make an evaluation of attainable intra-abdominal issues and strategically plan for object extraction either using conscious sedation on the bedside or underneath common anaesthesia in the working room. Radiographic research together with abdominal X-rays may determine whether the thing could be removed trans-anally or require laparotomy. If the thing could be eliminated trans-anally, intravenous sedation ought to be administered to allow relaxation of the stomach wall musculature as well as for affected person consolation. Injection of native anaesthetic into the anal sphincter may enable leisure of the sphincters and facilitate retrieval transanally. If this modality is unsuccessful, a lubricated Foley catheter could be handed cephalad to the thing, disrupting the vacuum seal proximal to the foreign body and the thing retrieved. If these makes an attempt fail, laparotomy could also be required to manually compress the rectum and squeeze the thing caudally through the rectum. Following retrieval of the thing, inflexible proctoscopy must be performed to evaluate the rectal mucosa for harm. Air insufflation of the rectum can identify any full thickness damage and direct applicable management. Isolated anal sphincter accidents could be repaired primarily with absorbable suture, especially if the injury is recognised quickly after it occurs. If the patient has different life-threatening accidents or if the presentation of the injury happens after 24 hours, delayed restore may be advisable. Military-related colon trauma is usually characterised by penetrating and damaging injuries, whereas civilian-related trauma is extra more doubtless to be blunt and non-destructive in nature. Grading scales developed for accidents of the colon and rectum have been developed which may help in management of those accidents. Surgical management associated problems of penetrating rectal accidents sustained in Iraq and Afghanistan. The administration of perforating accidents of the colon and rectum in civilian apply.
Lucipro 1000 mg buy discount online
If the perforation is localised antimicrobial rinse bad breath 500 mg lucipro cheap with amex, the sigmoid colon bearing the perforation is walled off by omentum antibiotic pills 750 mg lucipro order otc, small bowel, bladder, rectum, parietal peritoneum, and the genital tract in the feminine. Some of these sufferers will present with related obstruction, abscess, fistula or perforation. Many patients with atypical presentations of diverticulitis could have irritable bowel syndrome. Surgeons due to this fact must be facile with telling the distinction between both situations. Patients with free perforation will typically present with diffuse peritonitis and signs of systemic toxicity. Many sufferers will current with belly tenderness is usually related to some extent of belly distention. Right-sided tenderness can be a presentation in sufferers which have a redundant sigmoid colon that extends to the best side of the abdomen. Free perforation is associated with diffuse abdominal ache, generally referred pain within the shoulder and shortness of breath. Many patients typically describe modifications of their bowel habits corresponding to constipation, diarrhoea or an alternation in stool calibre. If current, rectal bleeding is extra suggestive of ischaemic colitis or inflammatory bowel disease. In complicated shows, an inflammatory phlegmon could be related to a small or giant bowel obstruction. Patients with an obstruction will current with abdominal distention and sometimes nausea and vomiting. Patients with fistulas could have minimal stomach complaints and may present initially to a urologist or gynaecologist. Patients who develop complications of diverticular disease corresponding to colovesical fistulas could current with pneumaturia, pyuria or faecaluria while sufferers with colovaginal fistulas may present with vaginal discharge, vaginal air or stool per vagina. The pain is usually persistent and boring, remaining constant over lengthy periods of time. Flat and upright plain films of the abdomen are generally obtained in the evaluation of the patient with acute abdominal ache to exclude obstruction or free intraperitoneal air. In sufferers with diverticular illness, the findings of plain movies tend to be non-specific. Contrast enemas are seldom currently used in the analysis and administration of diverticulitis. These indicators included the presence of diverticula, pericolic fat stranding, colonic wall thickening greater than 4 mm and abscess formation. Grade 1a consists of wall thickening and pericolonic fats stranding, whilst Grade 1b includes a pericolonic or mesocolic abscess. Patients with Grade 3 and Grade four disease have purulent and faecal peritonitis respectively. The presence of diverticulitis associated abscess was one explicit factor which was related to a excessive risk of failure with nonoperative administration. This strategy is mostly advocated to exclude the presence of a malignancy or another prognosis similar to ischaemic colitis or inflammatory bowel illness. This method is encouraged in order to keep away from potential conversion of a sealed microperforation right into a free perforation. Others have demonstrated that colonoscopy throughout an acute episode of diverticulitis may be protected. The presence of air in the urinary bladder within the absence of instrumentation is taken into account diagnostic. Colovesical fistulas are the commonest (65%), adopted by other forms of fistulas together with colovaginal, coloenteric, colouterine and colocutaneous fistulas. Patients often present with outstanding urinary signs including polymicrobial urinary tract infections, pneumaturia and faecaluria. If performed, cystoscopy exhibits inflammation generally at the dome of the bladder and, every so often, vegetable materials in the urine. Colovesical fistulas may be associated with domestically superior bladder or major colon cancer. Cystoscopy and colonoscopy may be appropriate to exclude a malignancy beneath applicable clinical circumstances. The surgical rules for remedy of colovesical fistulas because of diverticular illness embrace resection of the affected section of colon, almost all the time the sigmoid. Management of difficult diverticular disease is dependent on the particular presentation of the illness. Treatment of the issues of diverticulitis might range from treatment with bowel relaxation and parenteral antibiotics to emergent exploratory laparotomy. We will review the treatment choices for every of the complications of diverticulitis individually. A major anastomosis between the descending colon and the higher rectum can usually be performed safely. On event, non-operative management may be used for colovesical fistulas especially if the signs are minor and the patient has medical co-morbidities conferring a major operative danger. However, if non-operative treatment is advised, sufferers should be warned in regards to the potential lethal threat of urosepsis. Often, women have seen a gynaecologist initially for analysis of a vaginal discharge generally with gas. A single stage sigmoid resection with main anastomosis can typically be carried out, pinching off the positioning of the fistula from the top of the vaginal vault and interposing omentum. Diverticular Abscess Diverticular abscess occurs in roughly 10% to 25% of patients with acute diverticulitis. In ladies, an abscess related to a diverticula phlegmon might involve the adenexa resulting in tubo-ovarian abscess. Traditionally, patients with diverticulitis and an associated abscess have been handled by antibiotics and percutaneous drainage followed by interval elective sigmoid resection. This approach was primarily based on the remark that over 40% will develop recurrent sepsis. Abscesses lower than four cm in measurement often resolve with intravenous antibiotics alone without the need for additional procedures. A recent evaluate suggested 20% to 30% of diverticular abscesses have been amenable to percutaneous drainage and the failure fee of percutaneous drainage was 20% to 30%. Transabdominal drainage tends to be better tolerated when in comparability with different entry routes. In patients with easy unilocular abscesses, profitable drainage is achieved in approximately 80%. Patients with extra advanced abscesses related to loculations or fistula or when drainage route transverses regular organs are associated with a higher failure fee. The decision to perform a sigmoid resection following profitable drainage of a diverticular abscess must be approached on a case by case foundation.
Lucipro 250 mg mastercard
The majority of sufferers will need admission to either the excessive dependency or intensive care unit post-operatively antibiotics bad for you buy 750 mg lucipro otc. More than one senior surgeon and infrequently several surgical groups could additionally be required antibiotic prescribed for uti lucipro 250 mg discount amex, particularly when surgical procedure involves intensive reconstruction of each the gastrointestinal tract and stomach wall. Collaboration between colorectal, upper gastrointestinal, hepatobiliary, plastic and urological surgeons is commonly required for profitable completion of these procedures and, the place possible, must be totally deliberate in advance. Ureteric catheters are frequently required to have the ability to assist in identification of ureters, which are sometimes displaced on account of earlier pelvic surgery and tough to find in dense pelvic scar tissue. Entry into the stomach requires endurance and involves meticulous dissection so as to achieve this with out creating enterotomies. Once the entire small gut has been dissected free and measured, selections can be taken regarding intestinal resection and anastomosis. It ought to be famous, nonetheless, that although it could be easier to restore continuity when the distal section is atrophic by developing a side to facet (functional end to end) anastomosis, this will likely lead to lack of some absorptive surface Acute Intestinal Failure 1467 eighty one. The omentum (if available) could also be used to fill old abscess cavities by suturing it into place throughout the cavity, thus stopping the small gut and anastomosis from falling into the cavity. This can then be closed at a subsequent, smaller process, as soon as distal imaging has confirmed that the anastomoses have healed, probably after a interval of distal feeding. Small calibre intestinal anastomoses involving previously defunctioned bowel could end in a interval of intestinal obstruction. This must be anticipated and a drainage gastrostomy is a helpful adjunct to reconstructive surgery, as it avoids the need for prolonged nasogastric drainage. In distinction, an apparently giant defect may have a substantial amount of soft and pliable belly wall fascia at its margins and be amenable to dissection and primary suture restore. All contaminated prosthetic materials implanted at previous surgical procedure ought to be excised to minimise the chance of chronic infection and further fistulation. A single-stage strategy could additionally be appropriate in circumstances where there has been minimal or no lack of abdominal wall tissue. In some instances, it could be possible simply to pinch off the fistula, curette the monitor and shut the stomach in the ordinary way. The cutaneous opening of the fistula (by definition a contaminated wound) can also be curetted and then packed and left to heal by secondary intention. In bigger abdominal wall defects, the place a formal stomach wall reconstruction is repaired, the procedures might be undertaken at one sitting, or in a number of phases. Abdominal wall reconstruction is an important part of intestinal reconstructive surgical procedure, and it ought to by no means be underestimated. Polyglactin) to reconstruct the stomach wall, after which restore the abdominal wall defect with a non-absorbable prosthetic material at a later date, when the belly wall is not contaminated by the fistula. It is unclear whether a one-stage or multistage strategy to the restoration of gastrointestinal continuity and reconstruction of the abdominal wall is one of the best approach and both have potential benefits and drawbacks. Although a one-stage method avoids the need for several procedures, and their associated price and psychological morbidity, the outcome of a one-stage approach may be less passable, with reviews of recurrent fistulation in 26% and incisional hernia formation in 21%, after solely two years of follow-up. A second operation may be undertaken to cope with the resulting hernia a quantity of months later, underneath sterile circumstances, when the affected person has in any other case absolutely recovered. Biological implants are probably handiest when used at the side of autologous tissue reconstruction, and in particular with separation of components (see below). Whilst they can be used to bridge an abdominal wall defect, the speed of mechanical failure when used on this method has been unacceptably excessive, with incisional herniation occurring in as a lot as 80% of sufferers,100 and leaving cross-linked collagen in contact with the gastrointestinal tract has been reported to lead to recurrent fistulation in forty one. Autologous tissue may be used to reconstruct the abdominal wall and has the advantage of avoiding an infection in a surgical area, which is often already heavily contaminated. The available methods have been reviewed extensively74 and include separation of components101 and both pedicled102�105 and free flaps,106 with or with out the usage of biological implants placed between abdominal wall layers to reinforce closure of the stomach wall defect. In such cases, normally with stomach wall defects larger than 200 cm2 in floor space, substitute (effectively) of the abdominal wall utilizing a vascularised pedicled subtotal anterolateral flap based upon the lateral circumflex femoral artery may be useful. The higher and lower portions of the abdominal wall had been approximated, leaving the mesh in the middle. Acute Intestinal Failure 1469 stomach wall to get replaced, and with an affordable functional and beauty outcome. This is a fancy method with substantial morbidity, greatest suited to specialised centres. It is just applicable when used as part of a multistage reconstruction, because eighty one eighty one. There is, however, an increasing recognition that some sufferers with an anatomically passable size of small gut, however untreatable illness or irreversible obstruction of the small gut could lead to the identical nutritional and metabolic penalties, even if the small gut is normal in size per se. The size of the grownup small gut ranges from 275 to 850 cm and tends to be much less in women than in males. This may clarify why the majority (typically two-thirds) of patients with short bowel are girls. Patients who nonetheless have an intact colon appear to be comparatively protected and satisfactory nutritional, fluid and electrolyte standing has been described in individuals with as little as 30 to 50 cm of jejunum anastomosed to the colon. In general, sufferers with one hundred to 200 cm of jejunum in continuity with their colon are likely to want oral dietary supplements initially but finally achieve dietary autonomy. Some patients with 50 to 100 cm of small intestine anastomosed to colon will need long-term parenteral diet, and the vast majority of patients with less than 50 cm of jejunum anastomosed to the colon will need parenteral vitamin. All patients with lower than 30 cm of jejunum anastomosed to the colon will want long-term parenteral nutrition. The significance of the colon in fluid, electrolyte and power steadiness is demonstrated by the truth that most sufferers with less than 200 cm of small gut to an end jejunostomy will need parenteral fluid and sodium, and the majority of patients with less than a hundred cm of jejunum to an finish jejunostomy will require parenteral diet. Other elements which have been proven to have an result on survival embrace the size of remaining small intestine (patients with greater than a hundred cm of small gut have a considerably better prospect of surviving ten years than patients with less than 50 cm), and whether or not or not the colon is in continuity (10-year survival is nearly 50% higher if the colon is in continuity). Parenteral nutrition-related metabolic bone illness may develop, the trigger of which remains unclear, in addition to progressive liver dysfunction, which can develop all of a sudden after a few years of stability and apparently with out warning. Patients with small bowel dilatation (which may be maladaptive � see below) may be vulnerable to bacterial overgrowth and this will also contribute to abnormal liver function. Aggressive remedy of sepsis, discontinuation of hepatotoxic medication, adjustment of the nutritional regimen to limit glucose consumption, to increase the amount of omega-3�derived lipids and to promote using enteral feeding could also be of profit. The loss of bile salts related to resection of the distal small gut not only contributes to diarrhoea but also makes bile highly lithogenic. Those patients with an finish jejunostomy tend to have a lower urine output (at least during the day), which can leave them dehydrated and vulnerable to calculus formation because of the elevated focus of salts in urine. Patients with a jejunocolic anastomosis may theoretically be at threat of oxalate stones, because the malabsorption of fats in the shortened small bowel leaves stearate in the intestine to bind calcium salts. The oxalate is subsequently absorbed after which filtered within the urine, resulting in hyperoxaluria and calculus formation. The gut has appreciable capacity to adapt, even in adults, and there are a number of alterations in enterocyte kinetics, nutrient transporter gene expression, intestinal mass, villous height, crypt depth and intestinal diameter, all of which may promote larger effectivity of nutrient absorption. Whilst this will increase absorptive Chronic Intestinal Failure 1473 surface area, the increase in jejunal diameter can also result in stasis and bacterial overgrowth, making diarrhoea worse and potentially contributing to hepatocellular dysfunction.