Prasone
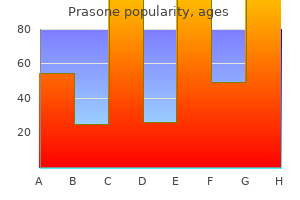
Prasone dosages: 40 mg, 20 mg, 10 mg, 5 mg
Prasone packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
These insulators are gene sequences that provide a barrier so that a specific gene is olated in opposition to transcriptional influences from surrounding genes allergy medicine empty stomach . A promoter is frequently managed by transcription elements situated elsewhere within the genome allergy testing cpt code . That is, the regulatory gene causes the formation of a regulatory protein that in flip acts either as an activator or a repressor of transcription. Occasionally, many different promoters are controlled on the same time by the identical regulatory protein. In some cases, the identical regulatory protein features as an activator for one promoter and as a repressor for an additional promoter. Even then, particular transcriptor components control the precise price of transcription by the promoter in the chromosome. The gene management techniques are particularly important for controlling intracellular concentrations of amino acids, amino acid derivatives, and intermediate substrates and products of carbohydrate, lipid, and protein metabolism. Thus, enzyme regulation represents a second category of mechanisms by which cellular biochemical functions can be controlled. Some chemical substances formed or inhibited, and likewise, the enzyme methods may be either activated or inhibited. However, on occasion, substances from without the cell (especially a few of the hormones discussed all through this text) additionally control the intracellular biochemical reactions by activating or inhibiting a number of of the intracellular management methods. Almost at all times the synthesized product acts on the first enzyme in a sequence, somewhat than on the next enzymes, normally binding instantly with the enzyme and causing an allosteric conformational change that inactivates it. The genes and their regulatory mechanisms determine the expansion traits of the cells and in addition when or whether these cells will divide to type new cells. In this way, the all-important genetic system controls each stage in the growth of the human being, from the singlecell fertilized ovum to the whole functioning physique. Enzymes which are usually inactive Life Cycle of the Cell the life cycle of a cell is the interval from cell copy to the following cell reproduction. It is terminated by a collection of distinct bodily events known as mitosis that trigger division of the cell into two new daughter cells. The actual stage of mitosis, nevertheless, lasts for under about 30 minutes, and thus greater than 95 percent of the life cycle of even quickly reproducing cells is represented by the interval between mitosis, called interphase. Except in particular situations of fast mobile copy, inhibitory elements virtually always sluggish or stop the uninhibited life cycle of the cell. Therefore, totally different cells of the body actually have life cycle durations that vary from as little as 10 hours for highly stimulated bone marrow cells to a whole lifetime of the human body for many nerve cells. Another attention-grabbing instance of each enzyme inhibition and enzyme activation happens in the formation of the purines and pyrimidines. When purines are formed, they inhibit the enzymes which are required for formation of extra purines. Conversely, the pyrimidines inhibit their own enzymes however activate the purine enzymes. This uncoiling is achieved by enzymes that periodically minimize every helix along its complete length, rotate every segment sufficient to cause separation, after which resplice the helix. Even throughout this period, preliminary changes that may result in the mitotic process are starting to happen. Because of repair and proofreading, errors are not often made within the transcription course of. The mutation causes formation of some irregular protein in the cell somewhat than a wanted protein, often resulting in abnormal cellular operate and sometimes even cell death. Yet on condition that 30,000 or more genes exist in the human genome and that the period from one human era to one other is about 30 years, one would anticipate as many as 10 or many extra mutations in the passage of the genome from father or mother to youngster. As an extra protection, nevertheless, each human genome is represented by two separate units of chromosomes with nearly similar genes. Therefore, one functional gene of each pair is type of all the time out there to the child despite mutations. Several nonhistone proteins are also major elements of chromosomes, functioning each as chromosomal structural proteins and, in reference to the genetic regulatory machinery, as activators, inhibitors, and enzymes. The two newly formed chromosomes stay hooked up to one another (until time for mitosis) at a degree called the centromere positioned close to their center. The complex of microtubules extending between the two new centriole pairs known as the spindle, and the complete set of microtubules plus the two pairs of centrioles is known as the mitotic apparatus. While the spindle is forming, the chromosomes of the nucleus (which in interphase include loosely coiled strands) turn into condensed into well-defined chromosomes. At the identical time, a quantity of microtubules from the aster connect to the chromatids on the centromeres, the place the paired chromatids are nonetheless sure to each other; the tubules then pull one chromatid of each pair towards one cellular pole and its companion towards the alternative pole. This pushing is believed to occur as a outcome of the microtubular spines from the 2 asters, where they interdigitate with each other to type the mitotic spindle, actually push one another away. Minute contractile protein molecules called "molecular motors, which are perhaps " composed of the muscle protein actin, extend between the respective spines and, using a stepping action as in muscle, actively slide the spines in a reverse direction along each other. Simultaneously, the chromatids are pulled tightly by their connected microtubules to the very middle of the cell, lining as much as form the equatorial plate of the mitotic spindle. All forty six pairs of chromatids are separated, forming two separate units of forty six daughter chromosomes. One of those sets is pulled towards one mitotic aster and the other is pulled toward the opposite aster as the 2 respective poles of the dividing cell are pushed nonetheless farther apart. Then the mitotic equipment dissolutes, and a model new nuclear membrane develops round every set of chromosomes. This membrane is fashioned from portions of the endoplasmic reticulum that are already present within the cytoplasm. This pinching is caused by formation of a contractile ring of microfilaments composed of actin and doubtless myosin (the two contractile proteins of muscle) on the juncture of the newly creating cells that pinches them off from each other. Once every chromosome has been replicated to kind the two chromatids, in lots of cells, mitosis follows automatically within 1 or 2 hours. One of the primary occasions of mitosis takes place in the cytoplasm; it happens in the course of the latter part of interphase in or across the small constructions known as centrioles. Each pair of centrioles, together with attached pericentriolar material, is recognized as a centrosome. Shortly before mitosis is to take place, the 2 pairs of centrioles begin to move aside from each other. This motion is brought on by polymerization of protein microtubules rising between the respective centriole pairs and truly pushing them apart. At the identical time, other microtubules develop radially away from each of the centriole pairs, forming a spiny star, referred to as the aster, in every end of the cell. Many other cells, however, such as clean muscle cells, might not reproduce for a number of years. In sure tissues, an insufficiency of some types of cells causes them to grow and reproduce quickly till applicable numbers of those cells are again obtainable.
Syndromes
- Loss of sensation around the nipple and areola
- Sodium hydroxide
- Behavior problems
- Secretin stimulation test for pancreas
- Chest pain
- What other home care aids do you use (toothpicks or other)?
- The doctor makes a small cut (incision) on your back. A needle is passed through the skin into your kidney.
- Fruit that has not been washed with clean water and then peeled
The lumbar plexus may be involved in retroperitoneal pathology allergy treatment non drowsy , and the sacral plexus may be invaded by pelvic malignancies allergy medicine you can take with zyrtec . Both may be concerned within the reticuloses, affected by plexiform neuromas, or damaged in fractures of the lumbar spine and pelvis or in different circumstances that trigger severe retroperitoneal and pelvic haemorrhage. Sciatica is ache in the decrease back and hip area, which radiates inferiorly along the posterior thigh to the leg. It is often brought on by a herniated intervertebral disc, compressing the L5 or S1 ventral rami. The so-called piriformis syndrome, which can end result from a variant or anomalous relationship between piriformis and the sciatic nerve, can also produce hip pain that radiates inferiorly along the course of the sciatic nerve. It arises from the posterior divisions of the second to fourth lumbar ventral rami, descends by way of psoas main and emerges on its lateral border to move between it and iliacus. It enters the thigh behind the inguinal ligament and lateral to the femoral sheath. Its terminal branches type in the femoral triangle about 2 cm distal to the inguinal ligament. In the abdomen, the nerve supplies small branches to iliacus and a department to the proximal part of the femoral artery. It subsequently provides a big cutaneous area on the anterior and medial thigh, medial leg and foot, and provides articular branches to the hip, knee and ankle. Obturatornerve(L2�4) the obturator nerve is the nerve of the medial compartment of the thigh. It arises from the anterior divisions of the second to fourth lumbar ventral rami, descends through psoas major and emerges from its medial border at the pelvic brim. It crosses the sacroiliac joint behind the frequent iliac artery and lateral to the internal iliac vessels, runs along the lateral pelvic wall medial to obturator internus, and enters the thigh through the higher a part of the obturator foramen. Near the foramen, it divides into anterior and posterior branches, which are separated at first by a half of obturator externus and more distally by adductor brevis. It provides articular branches to the hip and knee, and may provide skin on the medial thigh and leg. An accent obturator nerve may also be present and leaves the pelvis anterior to the pubis. Dorsal venous arch Sciaticnerve(L4,L5,S1�3) the sciatic nerve travels within the posterior compartment of the thigh and, via its major branches, supplies the leg and foot. It enters the lower limb by way of the higher sciatic foramen inferior to piriformis and descends between the higher trochanter and ischial tuberosity. Prior to diverging, the tibial and customary fibular nerves are structurally separate and only loosely held together as the sciatic nerve. The tibial nerve is derived from the anterior divisions of the sacral plexus, and the frequent fibular nerve is made up of the posterior divisions of the plexus. The sciatic nerve sends articular branches to the hip joint by way of its posterior capsule (these are sometimes derived instantly from the sacral plexus) and to the knee joint. The posterior thigh muscular tissues, including the ischial part of adductor magnus but not the brief head of biceps femoris, are supplied by the medial (tibial) part of the sciatic nerve. The short head of biceps femoris is supplied by the lateral (common fibular) element. The widespread variations of the sciatic nerve have been properly described and have been categorised into six sorts (Beason and Anson 1937). It descends obliquely along the lateral side of the popliteal fossa to the fibular head, lying between the tendon of biceps femoris and the lateral head of gastrocnemius; it then curves lateral to the neck of the fibula, lying on the bone deep to fibularis longus, and divides into superficial and deep fibular (peroneal) nerves. Before it divides, it provides branches to the knee and superior tibiofibular joints, and to the pores and skin. The cutaneous space supplied by the frequent fibular nerve and its terminal branches contains the anterolateral leg and most of the dorsum of the foot. External iliac nodes Deep inguinal nodes Superficial inguinal nodes Glutealnerves(L4,L5,S1,S2) the gluteal nerves arise from the posterior divisions of the sacral plexus. The superior gluteal nerve (L4, L5, S1) leaves the pelvis by way of the higher sciatic foramen superior to piriformis and provides gluteus medius, gluteus minimus, tensor fasciae latae and the hip joint. The inferior gluteal nerve (L5, S1, S2) passes by way of the higher sciatic foramen inferior to piriformis and supplies gluteus maximus. Variations in the composition and course of the cutaneous nerves of the decrease limb are frequent. Popliteal node Dermatomes Our knowledge of the extent of particular person dermatomes, especially in the limbs, is largely based mostly on medical evidence (Ladak et al 2014). Preganglionic sympathetic fibres to the lower limb are derived from neurones within the lateral horn of the lower thoracic (T10, T11 and T12) and upper lumbar (L1, L2) spinal cord segments. Fibres move in white rami communicantes to the sympathetic trunk and synapse within the lumbar and sacral ganglia. Postganglionic fibres move in gray rami communicantes to enter the lumbar and sacral plexuses; many are distributed to the pores and skin by way of the cutaneous branches of the nerves derived from these plexuses. The blood vessels to the decrease limb receive their sympathetic nerve provide through adjoining peripheral nerves. Postganglionic fibres accompanying the iliac arteries are destined primarily for the pelvis however may provide vessels within the proximal thigh. Tibialnerve(L4,L5,S1�3) the tibial nerve is derived from the anterior divisions of the sacral plexus. It descends along the posterior thigh and popliteal fossa to the distal border of popliteus, then passes anterior to the soleus with the popliteal artery and continues into the leg. In the popliteal fossa, it lies lateral to the popliteal vessels, becomes superficial to them at the knee and crosses to the medial aspect of the artery. It ends deep to the flexor retinaculum by dividing into the medial and lateral plantar nerves. Its cutaneous supply, including its terminal branches, provides the back of the calf, the solely real, the lateral border of the foot and the medial and lateral sides of the heel. The predominant segmental origin of the nerve provide for every of the muscular tissues of the lower limb and for the movements that happen on the joints of the decrease limb is summarized in Tables seventy eight. The ilioinguinal nerve may be a part of the iliohypogastric nerve on the iliac crest. When the obturator nerve makes a extra vital contribution to the cutaneous innervation, the medial cutaneous department of the femoral nerve is comparatively small. The lateral femoral cutaneous nerve normally arises from L2 and L3, however L1 may also contribute. Although it often bifurcates after it exits the pelvis, it may bifurcate throughout the pelvic cavity. The nerve may be absent on one aspect and/or could also be changed by the ilioinguinal nerve or a branch of the anterior femoral cutaneous nerve. The genital and femoral branches of the genitofemoral nerve might come up as separate offshoots of the lumbar plexus. The genital department might receive fibres from the twelfth thoracic nerve or may be completely absent, while the femoral branch could have an in depth distribution to the skin of the higher two-thirds of the thigh.
Uterine tube 2 Ovary Uterus 1 Ureter Uterine artery 3 Bladder Microstructure the vagina has an internal mucosal and an exterior muscular layer allergy juice recipe . There are two median longitudinal ridges on its epithelial floor: one anterior and the other posterior allergy symptoms mayo . Numerous transverse bilateral rugae prolong from these vaginal columns, divided by sulci of variable depth, giving an appearance of conical papillae. These transverse rugosities are most numerous on the posterior wall and near the orifice; they increase under the influence of oestrogen during puberty and being pregnant, are particularly well developed earlier than parturition, and decrease after the menopause (Corton 2012). The epithelium is non-keratinized, stratified, squamous just like, and continuous with, that of the ectocervix. After puberty, it thickens and its superficial cells accumulate glycogen, which provides them a transparent appearance in histological preparations. Natural vaginal bacteria, particularly Lactobacillus acidophilus, break down glycogen in the desquamated mobile debris to lactic acid. This produces a extremely acidic (pH 3) setting that inhibits the expansion of most different microorganisms. The quantity of glycogen is much less earlier than puberty and after the menopause, when vaginal infections are more frequent. Key: 1, distal ureter on the degree of the uterine artery; 2, dorsal to the infundibulopelvic ligament, near the pelvic bone; three, intramural portion of ureter on the angle of the vaginal cuff. The cells of the center and upper layers appear clear because of their glycogen content material. Abbreviations: A, anus; B, bladder; C, cervix; R, rectum; S, pubic symphysis; V, vagina; *, endometrium; **, inside myometrium of uterus (also known as the junctional zone); ***, outer myometrium of uterus. B, Abbreviations: O, ovaries; R, rectum; *, endometrium, **, inner myometrium of uterus (junctional zone); ***, outer myometrium of uterus. C, Abbreviations: B, bladder; C, cervix (which, from exterior to inner, has several layers, as seen on T2-weighted images: a high-signal-intensity outer cervical stroma (contiguous with the outer myometrium); a low-signal-intensity internal cervical stroma (contiguous with the inside myometrium); high-signal-intensity endocervical glands (contiguous with endometrium); and a really high-signal-intensity endocervical canal (contiguous with the endometrial canal)); R, rectum. D, Abbreviations: A, anus; I, ischio-anal fossa; S, pubic symphysis; U, urethra; V, vagina. The longitudinal fibres are continuous with the superficial muscle fibres of the uterus. A layer of unfastened connective tissue, containing in depth vascular plexuses, surrounds the muscle layers. The uterus is divided structurally and functionally into two main regions: the muscular physique of the uterus (corpus uteri) varieties the upper two-thirds, and the fibrous cervix (cervix uteri) varieties the decrease third. In 10�15% of girls, the entire uterus leans backwards at an angle to the vagina and is claimed to be retroverted. The spherical and ovarian ligaments are inferoanterior and inferoposterior, respectively, to every cornu. The fundus is in contact with coils of small gut and, sometimes, by distended sigmoid colon. The lateral margins of the physique are convex; on each side, their peritoneum is mirrored laterally to kind the broad ligament, which extends as a flat sheet to the pelvic wall 1294 Female reproductive system Table seventy seven. Neuroanatomy of the Female Abdominoplevic Region: A Review with Application to Pelvic Pain Syndromes. This usually happens at the degree of the interior os, probably the most inferior margin of the physique of the uterus. The vesicouterine pouch, between the bladder and uterus, is obliterated when the bladder is distended, however could additionally be occupied by small gut when the bladder is empty. The sigmoid colon, and occasionally the terminal ileum, lie posterior to the uterus. The cavity of the uterine body often measures 6 cm from the exterior os of the cervix to the wall of the fundus and is flat in its anteroposterior plane (Salardi et al 1985). Peritoneal folds the parietal peritoneum is mirrored over the upper genital tract to produce anterior (uterovesical), posterior (rectovaginal) and lateral peritoneal folds. Two longitudinal ridges, one each on its anterior and posterior walls, give off small, indirect, palmate folds that ascend laterally like the branches of a tree (arbor vitae uteri); the folds on opposing partitions interdigitate to shut the canal. In nonpregnant women, the isthmus undergoes menstrual adjustments, though these are much less pronounced than those occurring within the uterine physique. The external finish of the cervix enters the upper finish of the vagina, thereby dividing the cervix into supravaginal and vaginal parts. The supravaginal part is separated anteriorly from the bladder by cellular connective tissue: the parametrium, which also passes to the perimeters of the cervix and laterally between the 2 layers of the broad ligaments. The affected person is tilted head down in order that the small bowel is moved away from the uterus to give this view. The posterior or rectovaginal fold extends decrease than the anterior fold and consists of peritoneum mirrored from the posterior vaginal fornix on to the front of the rectum, thereby creating the deep recto-uterine pouch (pouch of Douglas). The recto-uterine pouch is bounded anteriorly by the uterus, supravaginal cervix and posterior vaginal fornix; posteriorly, by the rectum; and laterally, by the uterosacral ligaments. Between the ovary and uterine tube, the mesosalpinx incorporates vascular anastomoses between the uterine and ovarian vessels, the epoophoron and the paroophoron. It is connected to the hilum of the ovary and carries vessels and nerves to the ovary. The upper border is free and the lower border is steady with the peritoneum over the bladder, rectum and aspect wall of the pelvis. The borders are steady with one another at the free edge via the uterine fundus, and diverge below close to the superior surfaces of levatores ani. The broad ligament is split into an upper mesosalpinx, a posterior mesovarium and an inferior mesometrium. Mesometrium the mesometrium is the largest part of the broad ligament, and extends from the pelvic ground to the ovarian ligament and uterine physique. This ligament continues laterally over the external iliac vessels as a distinct fold. The mesometrium also encloses the proximal part of the spherical ligament of the uterus, as well as smooth muscle and loose connective tissue. Ligaments of the pelvis Round ligament the ligaments of the pelvis include the round, uterosacral, transverse cervical and pubocervical ligaments. Although conventionally described as ending in the labium majus, a cadaveric dissection examine found that, in ladies, the spherical ligament ended just exterior the exterior ring, with neither attachment nor extension to the caudal labium (the homologue of the hemiscrotum) (Attah and Hutson 1991). Near the uterus, the round ligament accommodates a considerable quantity of smooth muscle but this steadily diminishes and the terminal portion is solely fibrous. The spherical ligament additionally accommodates striated muscle, blood vessels, nerves and lymphatics. The latter drain the uterine region around the entry of the uterine tube to the superficial inguinal lymph nodes. In the fetus, a projection of peritoneum (processus vaginalis) is carried with the spherical ligament for a brief distance into the inguinal canal. A patent processus vaginalis within the inguinal canal in females is often referred to because the canal of Nuck; it might be asymptomatic or it could give rise to an inguinal hernia or hydrocele of the canal of Nuck. The round and ovarian ligaments both develop from the gubernaculum and are steady. The connective tissue lateral to the uterus and the cervix � the parametrium � continues down along the vagina because the paracolpium.
The lower panel reveals graphically the successive changes in membrane potential over a couple of 10 allergy testing using kinesiology ,000ths of a second allergy symptoms of low blood pressure , illustrating the explosive onset of the action potential and the just about equally rapid restoration. At this time, the membrane sud- denly turns into permeable to sodium ions, allowing super numbers of positively charged sodium ions to diffuse to the inside of the axon. The normal "polarized" state of -90 millivolts is instantly neutralized by the inflowing positively charged sodium ions, with the potential rising quickly in the optimistic direction-a course of known as depolarization. In giant nerve fibers, the good excess of optimistic sodium ions transferring to the inside causes the membrane potential to really "overshoot" beyond the zero degree and to turn out to be somewhat positive. Then, rapid diffusion of potassium ions to the outside re-establishes the normal unfavorable resting membrane potential, which is known as repolarization of the membrane. Within a few 10,000ths of a sec- brane potential before the action potential begins. A voltagegated potassium channel also performs an necessary function in rising the rapidity of repolarization of the membrane. These two voltage-gated channels are along with the Na+-K+ pump and the K+ leak channels. This channel has two gates-one near the outside of the channel known as the activation gate, and another near the within referred to as the inactivation gate. The upper left of the figure depicts the state of those two gates in the normal resting membrane when the membrane potential is -90 millivolts. In this state, the activation gate is closed, which prevents any entry of sodium ions to the interior of the fiber through these sodium channels. During this activated state, sodium ions can pour inward by way of the channel, rising the sodium permeability of the membrane as a lot as 500- to 5000-fold. During the resting state, the gate of the potassium channel is closed and potassium ions are prevented from passing by way of this channel to the exterior. When the membrane potential rises from -90 millivolts towards zero, this voltage change causes a conformational opening of the gate and permits elevated potassium diffusion outward through the channel. However, due to the slight delay in opening of the potassium channels, for essentially the most part, they open simply at the similar time that the sodium channels are starting to shut due to inactivation. Thus, the decrease in sodium entry to the cell and the simultaneous increase in potassium exit from the cell combine to pace the repolarization process, resulting in full restoration of the resting membrane potential inside another few 10,000ths of a second. The "Voltage Clamp" Method for Measuring the Effect of Voltage on Opening and Closing of the VoltageGated Channels. The same enhance in voltage that opens the activation gate additionally closes the inactivation gate. The inactivation gate, nonetheless, closes a number of 10,000ths of a second after the activation gate opens. That is, the conformational change that flips the inactivation gate to the closed state is a slower process than the conformational change that opens the activation gate. Therefore, after the sodium channel has remained open for a few 10,000ths of a second, the inactivation gate closes and sodium ions not can pour to the within of the membrane. At this point, the membrane potential begins to return towards the resting membrane state, which is the repolarization process. One of those electrodes is used to measure the voltage of the membrane potential, and the other is used to conduct electrical present into or out of the nerve fiber. This apparatus is used in the following means: the investigator decides which voltage to set up inside the nerve fiber. The electronic portion of the equipment is then adjusted to the specified voltage, automatically injecting either constructive or negative electricity by way of the current electrode at no matter price is required to maintain the voltage, as measured by the voltage electrode, at the level set by the operator. To counterbalance the effect of those ion movements on the specified setting of the intracellular voltage, electrical present is injected automatically via the current electrode of the voltage clamp to maintain the intracellular voltage at the required regular zero stage. To obtain this level, the current injected should be equal to but of reverse polarity to the net current flow via the membrane channels. Finally, the investigator adjusts the concentrations of the ions to aside from normal ranges both inside and out of doors the nerve fiber and repeats the study. This experiment may be performed easily when utilizing massive nerve fibers removed from some invertebrates, especially the enormous squid axon, which in some circumstances is as massive as 1 millimeter in diameter. When sodium is the only permeant ion in the options inside and outdoors the squid axon, the voltage clamp measures present circulate only via the sodium channels. When potassium is the only permeant ion, current flow solely through the potassium channels is measured. Another means for learning the circulate of ions by way of an individual sort of channel is to block one kind of channel at a time. Note the sudden opening of the sodium channels (the activation stage) within a small fraction of a millisecond after the membrane potential is elevated to the optimistic value. However, in the course of the next millisecond or so, the sodium channels mechanically shut (the inactivation stage). The bottom of the determine shows the modifications in membrane conductance for sodium and potassium ions. During the resting state, earlier than the motion potential begins, the conductance for potassium ions is 50 to a hundred times as great as the conductance for sodium ions. This disparity is brought on by a lot greater leakage of potassium ions than sodium ions through the leak channels. However, on the onset of the action potential, the sodium channels instantaneously become activated and permit up to a 5000-fold improve in sodium conductance. The inactivation course of then closes the sodium channels within another fraction of a millisecond. At the tip of the motion potential, the return of the membrane potential to the unfavorable state causes the potassium channels to close back to their unique standing, however again, solely after a further millisecond or more delay. During the early portion of the motion potential, the ratio of sodium to potassium conductance will increase more than 1000-fold. Therefore, far more sodium ions flow to the inside of the fiber than do potassium ions to the outside. This is what causes the membrane potential to become constructive at the action potential onset. Then the sodium channels start to close and the potassium channels begin to open, and thus the ratio of conductance shifts far in favor of excessive potassium conductance however low sodium conductance. This shift permits very rapid lack of potassium ions to the exterior but nearly zero flow of sodium ions to the interior. At least two other forms of ions should be considered: negative anions and calcium ions. They embody the anions of protein molecules and of many natural phosphate compounds, sulfate compounds, and so forth. The membranes of simply about all cells of the body have a calcium pump just like the sodium pump, and calcium serves along with (or as a substitute of) sodium in some cells to cause a lot of the motion potential. Like the sodium pump, the calcium pump transports calcium ions from the interior to the exterior of the cell membrane (or into the endoplasmic reticulum of the cell), creating a calcium ion gradient of about 10,000-fold. This course of leaves an internal cell focus of calcium ions of about 10-7 molar, in distinction to an external concentration of about 10-3 molar.
The lateral tibial condyle overhangs the shaft of the tibia posterolaterally above a small round facet for articulation with the fibula allergy forecast sugar land . In the sagittal plane allergy symptoms 8dpo , the articular surface is pretty flat centrally, and anteriorly and posteriorly the floor slopes inferiorly. Elsewhere, the floor has a raised medial margin that spreads to the lateral intercondylar tubercle. Its articular margins are sharp, besides posterolaterally, where the sting is rounded and easy: right here the tendon of popliteus is in contact with bone. Key: 1, posterior cruciate ligament; 2, tibial collateral ligament; three, medial meniscus; four, lateral meniscus; 5, fibular collateral ligament; 6, anterior cruciate ligament. A despair behind the base of the medial intercondylar tubercle is for the attachment of the posterior horn of the medial meniscus. The rest of the realm is easy and supplies attachment for the posterior cruciate ligament, spreading back to a ridge to which the capsule is attached. Femoral floor the femoral condyles, bearing articular cartilage, are virtually wholly convex. An various view is that the articular surface for contact with the tibia on the medial femoral condyle describes the arcs of two circles. According to this view, the anterior arc makes contact with the tibia close to extension and is part of a virtual circle of larger radius than the extra posterior arc, which makes contact during flexion. The lateral femoral condyle is believed to describe a single arc and thus to possess a single radius of curvature. Tibiofemoral congruence is improved by the menisci, that are formed to produce concavity of the surfaces introduced to the femur; the mixed lateral tibiomeniscal surface is deeper. The lateral femoral condyle has a faint groove anteriorly, which rests on the peripheral fringe of the lateral meniscus in full extension. The variations between the shapes of the articulating surfaces correlate with the movements of the knee joint. Anteromedially, anterior to the medial articular floor, a depression marks the positioning of attachment of the anterior horn of the medial meniscus. The anterior horn of the lateral meniscus is connected anterior to the intercondylar eminence, lateral to the anterior cruciate ligament. The eminence, with medial and lateral tubercles, is the narrow central a part of the area. The raised tubercles are thought to provide a slight stabilizing influence on the femur. It is believed that the eminence turns into outstanding as quickly as strolling commences and that the tibial condyles transmit the load of the physique via the tibia. The posterior horn of the lateral meniscus is hooked up to the posterior slope of the intercondylar space. The posterior intercondylar space inclines down and backwards behind the posterior horn of the lateral meniscus. They serve to widen, deepen and put together the tibial articular surfaces that receive the femoral condyles. Their peripheral hooked up borders are thick and convex, and their free, inner borders are thin and concave. Tears in the less vascular or inner zones seldom heal spontaneously; if surgery is indicated, these menisci are often resected. The meniscal horns are richly innervated in contrast with the remainder of the meniscus. The proximal surfaces are clean and concave, and in contact with the articular cartilage on the femoral condyles. The distal surfaces are smooth and flat, resting on the tibial articular cartilage. Canal-like constructions open on to the surface of the menisci in infants and young kids, and may transport vitamins to deeper, less vascular areas. The inside two-thirds of each meniscus encompass radially organized collagen bundles, and the peripheral one-third consists of bigger circumferentially arranged bundles (Ghadially et al 1983). Thinner collagen bundles parallel to the surface line the articular surfaces of the inner part, whereas the outer portion is roofed by synovium. This structural association suggests particular biomechanical capabilities for the 2 areas: the inner portion of the meniscus is suited to resisting compressive forces while the periphery is capable of resisting tensional forces. With ageing and degeneration, compositional modifications happen inside the menisci, which reduce their capability to resist tensional forces. Outward displacement of the menisci by the femoral condyles is resisted by agency anchorage of the peripheral circumferential fibres to the intercondylar bone at the meniscal horns. The menisci spread load by growing the congruity of the articulation, present stability by their physical presence and proprioceptive feedback, and should cushion the underlying bone from the appreciable forces generated during extremes of flexion and extension of the knee. In its mildest form, the partial discoid meniscus is simply a wider form of the normal lateral meniscus. A full discoid meniscus appears as a biconcave disc with a rolled medial edge and covers the lateral tibial plateau. The Wrisberg kind of meniscus has the identical form as an entire discoid meniscus but its only peripheral posterior attachment is by the meniscofemoral ligaments. In this case, the traditional tibial attachment of the posterior horn of the lateral meniscus is missing however the posterior meniscofemoral ligament persists. As a result, this kind of meniscus is attached anteriorly to the tibia and posteriorly to the femur, which renders the posterior horn unstable. However, they could trigger issue in gaining access to the lateral compartment at arthroscopy. Its exact function is conjectural, though one research discovered that the ligament was slightly taut in knee extension (Tubbs et al 2008); presumably, it helps to lower rigidity generated within the longitudinal circumferential fibres of the menisci when the knee is subjected to load. The anterior meniscofemoral ligament (ligament of Humphrey) passes anterior to the posterior cruciate ligament. The posterior meniscofemoral ligament (ligament of Wrisberg) passes behind the posterior cruciate ligament and attaches proximal to the margin of attachment of the posterior cruciate. It is connected by its anterior horn to the anterior tibial intercondylar area in entrance of the anterior cruciate ligament; the posterior fibres of the anterior horn are steady with the transverse ligament of the knee (when present). The anterior horn is in the floor of a depression medial to the higher part of the patellar ligament. The posterior horn is fixed to the posterior tibial intercondylar space, between the attachments of the lateral meniscus and posterior cruciate ligament. Its peripheral border is hooked up to the fibrous capsule and the deep surface of the tibial collateral ligament. Collectively, these attachments be sure that the medial meniscus is relatively fastened and strikes much less than the lateral meniscus.
Okra (Ambrette). Prasone.
- What is Ambrette?
- How does Ambrette work?
- Dosing considerations for Ambrette.
- Spasms, snakebites, stomach cramps, low appetite, headaches, stomach cancer, hysteria, gonorrhea, lung problems, and other conditions.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96064
The sequence of events nearly all the time begins with a preliminary streptococcal an infection triggered particularly by group A hemolytic streptococci allergy eye drops for dogs . These micro organism initially cause a sore throat allergy testing wheat , scarlet fever, or center ear infection. The antibodies react not only with the streptococcal protein but also with different protein tissues of the physique, often inflicting extreme immunologic harm. These reactions continue to happen as long as the antibodies persist within the blood-1 year or more. Rheumatic fever particularly causes injury in certain prone areas, such as the guts valves. The diploma of heart valve injury is instantly correlated with the concentration and persistence of the antibodies. In individuals with rheumatic fever, giant hemorrhagic, fibrinous, bulbous lesions develop along the infected edges of the heart valves. Because the mitral valve undergoes more trauma during valvular action than any of the opposite Other Causes of Valvular Lesions. Stenosis or lack of one or more leaflets of a valve also occurs occasionally as a congenital defect. Complete lack of leaflets is rare; congenital stenosis is extra frequent, as is discussed later on this chapter. Because of the resistance to ejection, generally the blood pressure in the left ventricle rises as high as 300 mm Hg, while the pressure within the aorta is still normal. Thus, a nozzle effect is created throughout systole, with blood jetting at large velocity through the small opening of the valve. This sound is harsh, and in persons with severe stenosis it could be so loud that it can be heard several ft away from the affected person. Also, the sound vibrations can typically be felt with the hand on the upper chest and lower neck, a phenomenon often identified as a thrill. This murmur results from turbulence of blood jetting backward into the blood already within the lowpressure diastolic left ventricle. In persons with mitral regurgitation, blood flows backward by way of the mitral valve into the left atrium throughout systole. As a end result, the sound of mitral regurgitation is transmitted to the chest wall primarily through the left ventricle to the apex of the center. Several important compensations happen that may ameliorate the severity of the circulatory defects. In each aortic stenosis and aortic regurgitation, the left ventricular musculature hypertrophies because of the elevated ventricular workload. In regurgitation, the left ventricular chamber additionally enlarges to maintain all the regurgitant blood from the aorta. Sometimes the left ventricular muscle mass will increase fourfold to fivefold, creating a tremendously large left side of the center. When the aortic valve is seriously stenosed, the hypertrophied muscle allows the left ventricle to develop as a lot as four hundred mm Hg of intraventricular stress at systolic peak. In individuals with severe aortic regurgitation, generally the hypertrophied muscle allows the left ventricle to pump a stroke volume output as great as 250 milliliters, though as a lot as three fourths of this blood returns to the ventricle during diastole, and only one fourth flows through the aorta to the physique. Another impact that helps compensate for the diminished net pumping by the left ventricle is elevated blood volume. This elevated quantity results from (1) an preliminary slight lower in arterial pressure, plus (2) peripheral circulatory reflexes induced by the decrease in strain. These mechanisms together diminish renal output of urine, inflicting the blood volume to improve and the mean arterial stress to return to normal. Also, purple blood cell mass finally increases due to a slight diploma of tissue hypoxia. The enhance in blood volume tends to increase venous return to the guts, which, in turn, causes the left ventricle to pump with the additional energy required to overcome the abnormal pumping dynamics. For this purpose, even in individuals with severe mitral stenosis, no murmur may be heard through the first third of diastole. Then, after partial filling, the ventricle has stretched enough for blood to reverberate and a low rumbling murmur begins. It is obvious from these phonocardiograms that the aortic stenotic lesion causes the loudest murmur, and the mitral stenotic lesion causes the weakest murmur. The phonocardiograms present how the intensity of the murmurs varies during totally different parts of systole and diastole, and the relative timing of every murmur can also be evident. This action will increase work load and oxygen consumption of the ventricle, necessitating elevated coronary blood circulate to ship this oxygen. The excessive wall tension of the ventricle, nonetheless, causes marked decreases in coronary flow during systole, significantly in the subendocardial vessels. With aortic regurgitation the intraventricular diastolic pressure additionally increases, compressing the inside layer of the guts muscle and reducing coronary blood circulate. Aortic diastolic strain decreases during aortic regurgitation, which might also decrease coronary blood move and cause ischemia of the heart muscle. In the early levels of aortic Aortic Valvular Lesions May be Associated with Inadequate Coronary Blood Flow. The buildup of blood in the left atrium causes progressive improve in left atrial pressure, finally resulting in the development of great pulmonary edema. This pathway could finally become so long that it predisposes to the development of excitatory signal circus actions, as discussed in Chapter thirteen. Therefore, in late stages of mitral valvular disease, especially in mitral stenosis, atrial fibrillation typically occurs. This growth additional reduces the pumping effectiveness of the guts and causes additional cardiac debility. As stenosis or aortic regurgitation, the intrinsic ability of the left ventricle to adapt to growing hundreds prevents significant abnormalities in circulatory operate in the person during relaxation, other than increased work output required of the left ventricle. Therefore, considerable degrees of aortic stenosis or aortic regurgitation often occur earlier than the person knows that she or he has serious heart disease (such as a resting left ventricular systolic strain as excessive as 200 mm Hg in individuals with aortic stenosis or a left ventricular stroke volume output as high as double regular in individuals with aortic regurgitation). As a consequence, the left ventricle dilates and cardiac output begins to fall; blood concurrently dams up in the left atrium and within the lungs behind the failing left ventricle. The left atrial pressure rises progressively, and at mean left atrial pressures above 25 to 40 mm Hg, serious edema seems in the lungs, as discussed in detail in Chapter 39. This increased blood quantity will increase venous return to the center, thereby helping to overcome the effect of the cardiac debility. Therefore, after compensation, cardiac output could fall only minimally until the late levels of mitral valvular disease, even though the left atrial strain is rising. As the left atrial stress rises, blood begins to dam up within the lungs, eventually all the way back to the pulmonary artery. In addition, incipient edema of the lungs causes pulmonary arteriolar constriction. These two effects collectively improve systolic pulmonary arterial strain and in addition right ventricular stress, typically to as excessive as 60 mm Hg, which is greater than double regular.
An in depth sarcoplasmic reticulum is current for speedy release of calcium ions to provoke contraction allergy shots natural . Large quantities of glycolytic enzymes are present for fast release of vitality by the glycolytic process allergy symptoms red ears . Fast fibers have a much less in depth blood supply than do gradual fibers because oxidative metabolism is of secondary significance. Fast fibers have fewer mitochondria than do slow fibers, also as a result of oxidative metabolism is secondary. Each motoneuron that leaves the more fully in Chapter eighty five on sports activities physiology, every muscle of the physique is composed of a mixture of so-called fast and sluggish muscle fibers, with still other fibers gradated between these two extremes. Muscles that react rapidly, including the anterior tibialis, are composed primarily of "fast" fibers with only small numbers of the slow variety. Conversely, muscle tissue corresponding to soleus that respond slowly but with extended contraction are composed primarily of "slow" fibers. The differences between these two types of fibers are described within the following sections. Compared with fast fibers, gradual fibers have a extra intensive blood vessel system and extra capillaries to supply additional quantities of oxygen. Slow fibers have greatly elevated numbers of mitochondria to assist excessive ranges of oxidative metabolism. In general, small muscle tissue that react rapidly and whose control have to be precise have extra nerve fibers for fewer muscle fibers (for occasion, as few as two or three muscle fibers per motor unit in a number of the laryngeal muscles). An average determine for all the muscles of the physique is questionable, but an excellent guess would be about eighty to 100 muscle fibers to a motor unit. This interdigitation allows the separate motor items to contract in support of one another rather than entirely as particular person segments. Summation means the including collectively of particular person twitch contractions to increase the intensity of overall muscle contraction. Summation occurs in two ways: (1) by rising the number of motor items contracting concurrently, which is known as a number of fiber summation, and (2) by rising the frequency of contraction, which is recognized as frequency summation and might result in tetanization. When the central nervous system sends a weak sign to contract a muscle, the smaller motor units of the muscle may be stimulated instead of the larger motor items. Then, because the power of the sign will increase, larger and larger motor units start to be excited as properly, with the biggest motor items often having as much as 50 times the contractile pressure of the smallest items. This phenomenon, referred to as the scale principle, is necessary because it allows the gradations of muscle pressure during weak contraction to happen in small steps, whereas the steps turn into progressively larger when massive amounts of force are required. Another necessary characteristic of multiple fiber summation is that the totally different motor models are pushed asynchronously by the spinal wire; consequently, contraction alternates among motor units one after the opposite, thus providing clean contraction even at low frequencies of nerve indicators. Individual twitch contractions occurring one after another at low frequency of stimulation are displayed to the left. Then, as the frequency will increase, there comes some extent when each new contraction occurs before the preceding one is over. As a result, the second contraction is added partially to the first, and thus the entire power of contraction rises progressively with rising frequency. When the frequency reaches a important level, the successive contractions finally turn into so fast that they fuse together and the entire muscle contraction seems to be completely clean and steady, as proven in the figure. At a barely greater frequency, the power of contraction reaches its maximum, and thus any extra increase in frequency beyond that point has no further effect in rising contractile force. Tetany happens because enough calcium ions are maintained within the muscle sarcoplasm, even between motion potentials, in order that full contractile state is sustained with out allowing any rest between the motion potentials. The maximum power of tetanic contraction of a muscle operating at a traditional muscle length averages between 3 and four kilograms per square centimeter of muscle, or 50 pounds per sq. inch. Because a quadriceps muscle can have up to sixteen square inches of muscle stomach, as a lot as 800 kilos of pressure could also be applied to the patellar tendon. Changes in Muscle Strength at the Onset of Contraction-The Staircase Effect (Treppe). When a muscle begins to contract after an extended interval of relaxation, its initial strength of contraction may be as little as one half its strength 10 to 50 muscle twitches later. That is, the power of contraction increases to a plateau, a phenomenon called the staircase effect, or treppe. Even when muscles are at relaxation, a particular amount of tautness usually remains, which is recognized as muscle tone. These nerve impulses, in turn, are managed partly by alerts transmitted from the mind to the suitable spinal wire anterior motoneurons and partly by alerts that originate in muscle spindles situated in the muscle itself. Both of these alerts are mentioned in relation to muscle spindle and spinal cord operate in Chapter 55. Studies in athletes have proven that muscle fatigue will increase in nearly direct proportion to the speed of depletion of muscle glycogen. Therefore, fatigue outcomes mainly from incapability of the contractile and metabolic processes of the muscle fibers to proceed supplying the identical work output. However, experiments have also shown that transmission of the nerve signal through the neuromuscular junction, which is discussed in Chapter 7, can diminish no less than a small amount after intense extended muscle activity, thus additional diminishing muscle contraction. Interruption of blood circulate through a contracting muscle leads to nearly full muscle fatigue inside 1 or 2 minutes because of the loss of nutrient supply, particularly the lack of oxygen. Muscles operate by making use of tension to their factors of insertion into bones, and the bones in flip form various types of lever methods. If we assume that a large biceps muscle has a cross-sectional space of 6 sq. inches, the utmost pressure of contraction would be about 300 pounds. When the forearm is at proper angles with the upper arm, the tendon attachment of the biceps is about 2 inches anterior to the fulcrum at the elbow, and the entire length of the forearm lever is about 14 inches. Therefore, the amount of lifting energy of the biceps on the hand would be only one seventh of the 300 kilos of muscle drive, or about forty three pounds. When the arm is totally extended, the attachment of the biceps is much lower than 2 inches anterior to the fulcrum, and the drive with which the hand could be brought ahead can be a lot less than 43 kilos. In brief, an evaluation of the lever systems of the physique is dependent upon data of (1) the point of muscle insertion, (2) its distance from the fulcrum of the lever, (3) the length of the lever arm, and (4) the place of the lever. Many types of movement are required in the body, some of which need great strength and others of which want massive distances of movement. For this cause, there are lots of different types of muscle; some are long and contract an extended Fulcrum Biceps muscle Lever Muscle Fatigue. The study of various kinds of muscular tissues, lever techniques, and their movements is called kinesiology and is a vital scientific part of human physioanatomy. Virtually all physique actions are attributable to simultaneous contraction of agonist and antagonist muscle tissue on reverse sides of joints. The position of each separate part of the physique, such as an arm or a leg, is determined by the relative levels of contraction of the agonist and antagonist units of muscle tissue. For instance, allow us to assume that an arm or a leg is to be positioned in a midrange place.
The perforators that provide the anteromedial thigh are derived from the femoral artery allergy testing kirkland wa , and those for the anterolateral thigh are derived from branches of the lateral circumflex femoral artery allergy forecast hollywood fl . Perforators that supply the pores and skin over the posteromedial and posterolateral thigh areas are derived from the profunda femoris artery and the popliteal arteries. Skin flaps based on the superficial circumflex iliac, superficial external pudendal and superficial inferior epigastric arteries have been used as local flaps, tube pedicles and free tissue transfers. The vein occupies the center compartment of the femoral sheath, between the femoral artery and femoral canal; fat in the canal permits growth of the vein. The profunda femoris vein (deep vein of the thigh, deep femoral vein) joins the femoral vein posteriorly 4�12 cm distal to the inguinal ligament, and the long saphenous vein then enters anteriorly. Veins accompanying the superficial epigastric, superficial circumflex iliac and exterior pudendal arteries be part of the lengthy saphenous vein earlier than it enters the saphenous opening. Lateral and medial circumflex femoral veins are normally tributaries of the femoral vein. There are often four or 5 valves within the femoral vein; the 2 most constant are just distal to the entry of profunda femoris and near the inguinal ligament. Anastomoses on the back of the thigh An important chain of anastomoses extends on the back of the thigh from the gluteal region to the popliteal fossa. The trochanteric and cruciate anastomoses are the proximal parts of this chain. Branches from this ring, the retinacular vessels, pierce the capsule and ascend alongside the femoral neck to give the principle blood supply to the top of the femur. Profunda femoris vein (Deep vein of the thigh) cruciate anastomosis the cruciate anastomosis lies on the degree of the lesser trochanter, close to the lower fringe of the femoral attachment of quadratus femoris, and is an anastomosis between the transverse branches of the medial and lateral circumflex femoral arteries, a descending department of the inferior gluteal artery and an ascending department from the primary perforating artery. Profunda femoris lies anterior to its artery and receives tributaries comparable to the branches of the artery. Through these tributaries it connects distally with the popliteal vein and proximally with the inferior gluteal veins. It sometimes drains the medial and lateral circumflex femoral veins and has a valve simply earlier than it empties into the femoral vein. Long saphenous vein Collateral circulation in proximal femoral artery occlusion 1370 After occlusion of the femoral artery proximal to the origin of the profunda femoris artery, 5 main anastomotic channels are available. These are between branches of the superior and inferior gluteal arteries, the medial and lateral circumflex femoral arteries and the first perforating department of the profunda femoris artery; the obturator branch of the internal iliac artery and the medial circumflex femoral artery; the inner pudendal branch of the internal iliac artery and the superficial and deep exterior pudendal branches of the femoral artery; a deep circumflex iliac branch of the exterior iliac artery, the lateral circumflex femoral branch of the deep artery of the thigh and the superficial circumflex iliac department of the femoral artery; and the inferior gluteal department of the inner iliac artery and perforating branches of the profunda femoris artery. It ascends immediately anterior to the tibial malleolus, crosses the distal third of the medial floor of the tibia obliquely in an anteroposterior course to reach its medial border, after which ascends a little behind the border to the knee. Section 9 innervation In its course through the thigh, the long saphenous vein is accompanied by the medial branches of the anterior cutaneous branches of the femoral nerve. At the knee, the saphenous department of the descending genicular artery (the saphenous artery) and, within the leg and foot, the saphenous nerve all lie anterior to the vein. One is current simply earlier than the vein pierces the cribriform fascia, one other at its junction with the femoral vein. In almost its entire extent the vein lies in subcutaneous tissue, but it has many connections with the deep veins, particularly in the leg. They receive all the superficial vessels of the lower limb, besides those from the posterolateral calf. All superficial inguinal nodes drain to the external iliac nodes, some by way of the femoral canal and others anterior or lateral to the femoral vessels. Superficial inguinal nodes are frequently enlarged in disease or harm in their region of drainage. Thus the proximal inguinal nodes are virtually invariably affected in malignant or infective disease of the prepuce, penis, labia majora, scrotum, perineum, anus and lower vagina, or in illnesses affecting the pores and skin and superficial constructions in these regions, within the infra-umbilical a part of the abdominal wall or in the gluteal area. In the leg, it typically connects with the brief saphenous vein and with deep veins via perforating veins. This vein was first illustrated by Leonardo da Vinci, whose name is typically given to it. It connects with posterior tibial venae comitantes by a collection of perforating (communicating) veins. There are often three, equally spaced between the medial malleolus and the mid-calf. More than three such perforators are uncommon, and an arch vein perforator above mid-calf is just very rarely found. Above the posterior crural arch vein, perforating veins join the lengthy saphenous vein or considered one of its major tributaries at two primary sites. The first is at a degree within the higher calf indicated by its name, the tibial tubercle perforator; the second is in the lower/intermediate third of the thigh, the place it perforates the deep fascia roof of the subsartorial canal to be a part of the femoral vein. Some open independently, while others converge to form massive named channels that frequently pass in direction of the basal half of the femoral triangle before becoming a member of the long saphenous close to its termination. These may be grouped as follows: a number of giant posteromedial tributaries, a number of massive anterolateral tributaries, and four or extra periinguinal veins. The posteromedial vein of the thigh, massive and typically double, drains a big superficial area indicated by its name; it has (as have the opposite tributaries) radiological and surgical significance. The posteromedial vein is usually named the accessory saphenous vein, though some restrict the time period accessory to a decrease (more distal) posteromedial tributary when two (or more) are current. Another large vessel, the anterolateral vein of the thigh (anterior femoral cutaneous vein), normally commences from an anterior network of veins in the distal thigh and crosses the apex and distal half of the femoral triangle to attain the long saphenous vein. Superficial epigastric and circumflex iliac veins drain the inferior belly wall, the latter additionally receiving tributaries from the proximolateral region of the thigh. The superficial epigastric or the femoral vein may connect with the lateral thoracic veins via a thoracoepigastric vein that runs superficially on the anterolateral side of the trunk. This vein connects the inferior and superior caval areas of drainage and may be dilated and visible in cases of inferior caval obstruction. Superficial exterior pudendal veins drain a half of the scrotum/labia; one is joined by the superficial dorsal vein of the penis/ clitoris. The deep exterior pudendal veins be part of the lengthy saphenous vein at the saphenous opening. The long saphenous vein is often harvested for grafts utilized in both peripheral and coronary arterial surgery. Deep inguinal nodes the deep inguinal nodes vary from one to three, and are located medial to the femoral vein. One lies simply distal to the saphenofemoral junction, one other in the femoral canal, and probably the most proximal node lies laterally in the femoral ring. All obtain deep lymphatics that accompany the femoral vessels, lymph vessels from the glans penis or clitoris and some efferents from the superficial inguinal nodes. The iliohypogastric, ilioinguinal and genitofemoral nerves are described on pages 1094�1096.

Vulvar nerves are prone to trauma and inflammation allergy symptoms to kefir , leading to food allergy treatment 2013 vulvar ache syndromes or vulvodynia (Shoja et al 2013). The deep inguinal nodes drain through the femoral canal to the pelvic nodes Table 77. Lymph vessels within the perineum and decrease a half of the labia majora drain to the rectal lymphatic plexus. Prepubertal distal longitudinal folds are frequent inside the vagina and so they disappear throughout puberty (Altchek et al 2008). The uterine, inner pudendal and center rectal branches of the internal iliac artery could contribute to the blood supply of the vagina. The hymen is a thin fold of mucous membrane located simply throughout the vaginal orifice. The inside surfaces of the folds are usually in contact with each other and the vaginal opening appears as a cleft between them. The hymenal ring usually ruptures after first sexual intercourse, however can rupture earlier throughout non-sexual bodily exercise. Small spherical carunculae hymenales (also often known as carunculae myrtiformis) are its remnants Veins the vaginal veins, one on both sides, come up from lateral plexuses that join with uterine, vesical and rectal plexuses and drain to the interior iliac veins. The uterine and vaginal plexuses could present collateral venous drainage to the lower limb. Lymphatic drainage Vaginal lymphatic vessels link with these of the cervix, rectum and vulva. Upper vessels accompany the uterine artery to the inner and external iliac nodes; intermediate vessels accompany the vaginal artery to the internal iliac nodes; and vessels draining the vagina beneath the hymen, and from the vulva and perineal pores and skin, cross to the superficial inguinal nodes (see Table seventy seven. Lower genital tract Innervation the decrease vagina is supplied by the pudendal nerve (S2, S3 and S4). Abdominal aorta Ovarian artery Developmental anomalies of the vagina Congenital anomalies of the vagina are vaginal agenesis, absent hymen, transverse vaginal septum and persistent cloaca. Vaginal agenesis, in the presence of different M�llerian duct anomalies and renal agenesis, is termed Mayer�Rokistansky�Kuster�Hauser syndrome. An absent hymen in sufferers with vaginal agenesis is associated with renal agenesis (Kimberley et al 2012). A congenital transverse septum could additionally be present throughout the vagina and manifests clinically in adolescence with main amenorrhoea and haematocolpos. Children with a persistent cloaca have a congenital defect characterized by fusion of the rectum, vagina and urethra into a single widespread channel that varies in length from 1 to 7 cm. They pass again from the cervix and uterine body on both sides of the rectum, and are hooked up to the anterior side of the sacrum. They could be palpated laterally on rectal examination and may be felt as thick bands of tissue passing downwards on either side of the posterior fornix on vaginal examination. The lower parts of the ureters and pelvic blood vessels traverse the transverse cervical ligaments. Fibres of the pubocervical ligament pass forwards from the anterior facet of the cervix and upper vagina to diverge across the urethra, and are connected to the posterior side of the pubic bones. The transverse cervical and uterosacral ligaments are virtually vertically orientated within the standing place and maintain the nearFundus of uterus Ovary and tube Anastomosis of ovarian and uterine vessels Ovarian artery and vein Mesosalpinx horizontal axis of the higher vagina. The uterus and vagina are supported by the shut interaction of the uterosacral and transverse cervical ligaments with the muscles of the pelvic ground, including the levatores ani and coccygei, the perineal membrane and the perineal body. The help of the pelvic flooring has been reviewed in detail by Delancey (2011) (see additionally Ch. One major branch ascends the uterus tortuously within the broad ligament till it reaches the area of the ovarian hilum, where it anastomoses with branches of the ovarian artery. Another branch descends to supply the cervix and anastomoses with branches of the vaginal artery to kind two median longitudinal vessels: the azygos arteries of the vagina, which descend anterior and posterior to the vagina. Although there are anastomoses with the ovarian and vaginal arteries, the dominance of the uterine artery is indicated by its marked hypertrophy throughout being pregnant. The tortuosity of the vessels as they ascend in the broad ligaments is repeated in their branches within the uterine wall. These enter the uterine wall, divide and run circumferentially as teams of anterior and posterior arcuate arteries. They ramify and slim as they approach the anterior and posterior midline in order that no giant vessels are current in these regions. However, the left and right arterial trees anastomose across the midline and unilateral ligation could be performed with out severe effects. Terminal branches in the uterine muscle are tortuous and are referred to as helicine arterioles. They present a series of dense capillary plexuses in the myometrium and endometrium. From the arcuate arteries, many helical arteriolar rami move into the endometrium. In the proliferative phase, helical arterioles are much less outstanding, whereas they grow in length and calibre, changing into much more tortuous in the secretory section. Broad ligament Uterine artery and vein Ureter Veins Vagina the uterine veins extend laterally in the broad ligaments, running adjoining to the arteries and passing over the ureters. The uterine venous plexus anastomoses with the vaginal and ovarian venous plexuses. The obturator nodes lie in the obturator fossa between the external and inner iliac vessels; the obturator nerve passes through the lower a part of this group of lymph nodes. The area surrounding the isthmus of the uterine tube may drain alongside the spherical ligament to the superficial inguinal nodes. They supply the uterine body and tubes, and connect with tubal nerves from the inferior hypogastric plexus and with the ovarian plexus. The uterine nerves terminate within the myometrium and endometrium, and normally accompany the vessels (see Table 77. Branches may move on to the cervix uteri or may be distributed along the vaginal arteries. Efferent preganglionic sympathetic fibres are derived from neurones within the final thoracic and first lumbar spinal segments; the sites the place they synapse on their postganglionic neurones are unknown however are presumably within the superior and/or inferior hypogastric plexuses (Lee et al 1973). Preganglionic parasympathetic fibres arise from neurones within the second to fourth sacral spinal segments and relay within the paracervical ganglia. Sympathetic activity may produce uterine contraction and vasoconstriction, and parasympathetic exercise might produce uterine inhibition and vasodilation, but these actions are difficult by hormonal management of uterine functions. The endometrium is formed by a layer of connective tissue, the endometrial stroma, which supports a single-layered columnar epithelium. It incorporates glands which are composed largely of columnar cells secreting glycoproteins and glycogen. After puberty, the construction of the endometrium varies with the stage of the menstrual cycle (see below).
They are additionally active during flexion (longus) and extension (magnus) of the thigh on the hip joint allergy testing boston . Testing of the adductors the adductors are often tested as a group by adduction of the thigh against resistance peanut allergy treatment 2013 , in the supine position with the knee extended. The tendon of adductor magnus could be felt simply proximal to the adductor tubercle on the medial condyle of the femur. It arises from the pecten pubis, from the bone anterior to it between the iliopubic ramus and the pubic tubercle, and from the fascia by itself anterior floor. The fibres descend, initially posteromedially and then posterolaterally, to be connected along a line from the lesser trochanter to the linea aspera. Proximally, it could be partially or wholly connected to the capsule of the hip joint. Vascular supply the primary arterial provide to pectineus is derived from the medial circumflex femoral artery, which enters the superficial floor of the muscle. There could also be a department from the femoral artery more proximally, and a deep supply from the obturator artery. Innervation Pectineus is innervated by the femoral nerve, L2 and 3, and the accessory obturator nerve, L3 (when present). The muscle may be incompletely divided into dorsal and ventral layers, that are provided by the obturator and femoral (or not often, accent obturator) nerves, respectively. Relations Pectineus is expounded anteriorly to the deep lamina of the fascia lata, which separates it from the femoral vessels and lengthy saphenous vein; posteriorly, to the capsule of the hip joint, adductor brevis, obturator externus and the anterior department of the obturator nerve; Actions Pectineus adducts the thigh and flexes it on the pelvis. Inferomedially, the tendinous fibres intermingle to some extent with those of biceps femoris and semitendinosus. The tendon receives, from the ischial tuberosity and ramus, two fibrous expansions that flank adductor magnus. It then broadens and descends deep to semitendinosus and the lengthy head of biceps femoris. Muscle fibres come up from the tendon at about mid-thigh and converge to a second aponeurosis on the posterior aspect of the lower a part of the muscle, which tapers to the heavy, rounded tendon of the distal attachment. The primary one is connected to a tubercle (sometimes called the tuberculum tendinis) on the posterior aspect of the medial tibial condyle. The others are: a collection of slips to the medial margin of the tibia, immediately behind the tibial collateral ligament; a thin fibrous growth to the fascia over popliteus; a cord-like tendon to the inferior lip and adjoining a part of the groove on the again of the medial tibial condyle, deep to the tibial collateral ligament; and a strong growth that passes obliquely upwards to the femoral intercondylar line and lateral femoral condyle, and types much of the oblique popliteal ligament of the knee joint. It begins at the apex of the femoral triangle and extends distally as far as the distal attachment of the tendon of adductor magnus. It is triangular in part and is bounded anterolaterally by vastus medialis; posteromedially by adductor longus; and distal to adductor longus, by adductor magnus. Its anteromedial boundary (often referred to as the roof) is a powerful and dense fascia that extends from the medial surface of vastus medialis to the medial fringe of the adductors longus and magnus, overlapping in its stride the femoral vessels in the adductor canal. This fascia, on account of being overlain by sartorius, is termed the subsartorial fascia. The adductor canal incorporates the femoral artery and vein, the descending genicular and muscular branches of the femoral artery and their corresponding venous tributaries, the saphenous nerve, and the nerve to vastus medialis (until it enters its muscle). The femoral vessels pass from the adductor canal into the popliteal fossa by way of the adductor hiatus, an opening within the tendon of adductor magnus adjoining to the femoral shaft, two-thirds of the way down the adductor canal. They cross both hip and knee joints, and integrate extension on the hip with flexion on the knee. As the muscle tissue span the back of the knee, they type the proximal lateral and medial margins of the popliteal fossa. This vessel has essential anastomoses with the inferior gluteal artery (on or inside semitendinosus) and with the medial circumflex femoral artery, while the third perforator anastomoses with the superior medial genicular artery throughout the quick head of biceps femoris. This anastomotic chain types an essential collateral arterial pathway when the femoral artery is blocked. The distal end of the muscle partially overlies the medial head of gastrocnemius earlier than passing anteromedially to it. An necessary bursa lies between the semimembranosus tendon and gastrocnemius, and sometimes communicates with the knee joint and with a smaller bursa between the tendon and the posterior tibial margin. Vascular provide Semimembranosus is equipped from the perforating arteries, normally from all, although predominantly from the first. A department of the femoral or popliteal artery supplies the distal a part of the muscle, and there could additionally be a contribution from the inferior gluteal artery at the proximal attachment. Innervation Semimembranosus is innervated by the sciatic nerve, L5, S1 and 2, by way of its tibial division. The belly is fusiform and ends a little beneath mid-thigh in a protracted, rounded tendon that runs on the posterior floor of semimembranosus. A tendinous intersection is often current close to the midpoint of the muscle, which can additionally receive a muscular slip from the long head of biceps femoris. These connections with the medial head of gastrocnemius and biceps femoris could cause difficulty when harvesting the tendon surgically for a graft. The relations of the distal part of the muscle are described above and with the pes anserinus. Semitendinosus Vascular supply the two primary arteries of provide to semitendinosus are superior and inferior. The superior is derived from both the medial circumflex femoral artery or the primary perforating artery. The inferior and bigger branch arises from the primary perforator distal to the origin of the superior department. An accent provide on the ischial attachment is derived from the inferior gluteal artery, and on the tibial attachment from the inferior medial genicular artery. The different, the short head, arises from the lateral lip of the linea aspera, between adductor magnus and vastus lateralis. This attachment extends proximally virtually to gluteus maximus and distally alongside the lateral supracondylar line to inside 5 cm of the lateral femoral condyle, and from the lateral intermuscular septum. The lengthy head varieties a fusiform belly that descends laterally throughout the sciatic nerve. This aponeurosis receives on its deep floor the fibres of the short head, and gradually narrows to a tendon (the lateral hamstring). The main part of the tendon splits around the fibular collateral ligament and is connected to the pinnacle of the fibula. The intermediate lamina fuses with the fibular collateral ligament, whereas the others cross superficial and deep to the ligament to attach to the lateral condyle of the tibia. Additional slips could arise from the ischial tuberosity, linea aspera or medial supracondylar line. Relations Proximally, biceps femoris is roofed by gluteus maximus, but elsewhere it lies relatively superficially. Deep to it lie semimembranosus proximally, and the sciatic nerve, adductor magnus and the lateral head of gastrocnemius more distally. The widespread fibular nerve descends along the medial border of the tendon of biceps femoris, separating it distally from the lateral head of gastrocnemius. The widespread fibular nerve is found rising posterior to the biceps femoris tendon, which is a helpful information to finding the nerve and avoiding iatrogenic injury. The nerve is adherent to the tendon; if part of the fibular head or the attachment of the tendon of biceps femoris, usually with the insertion of the fibular collateral ligament, is avulsed, then the tendon will exert proximal traction on the nerve, which can contribute to widespread fibular nerve traction damage.