Rulide
Rulide dosages: 150 mg
Rulide packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

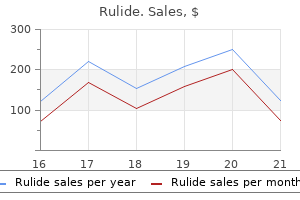
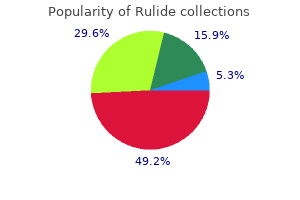
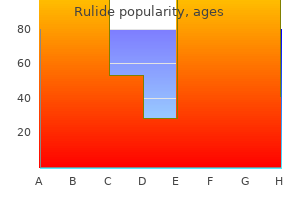
Discount 150 mg rulide mastercard
Preoperative planning ought to think about using stemmed implants medicine 319 discount 150mg rulide overnight delivery, which may complicate extraction of the component symptoms diabetes type 2 purchase rulide 150 mg. Metal slicing burrs and discs could also be necessary to separate the condylar portion of the femoral implant or the keel portion of the tibial implant from the stem. Some corporations might make special extraction gadgets out there to assist in elimination of the stem. Rarely, it could be essential to perform an osteotomy to extract significantly tough stems. Intraoperative approach Excellent exposure have to be achieved to keep away from iatrogenic bone and delicate tissue injury. The extensor mechanism should be handled with care to keep away from avulsion of the patella tendon insertion. Stemmed implants may require special instrumentation, metal-cutting burrs or discs, or ultrasonic instruments to remove. Bone loss Fracture Ligament disruption Tendon disruption Chapter 26 Revision Total Knee Arthroplasty With Extensile Exposure: Tibial Tubercle Osteotomy Anish K. The options obtainable for coping with troublesome publicity include extensor mechanism snip (done 5 to 8 cm proximal to the superior pole of the patella), V-Y quadriceps turndown, and tibial tubercle osteotomy. An osteoperiosteal segment-which includes the tibial tubercle and upper tibial crest-is elevated to chill out the extensor mechanism and permit safe eversion of the patella. A medial parapatellar arthrotomy, mixed with intraarticular excision of the fibrous pseudocapsule, permits eversion of the patella generally. Inadequate exposure with continued forceful retraction of the extensor mechanism dangers avulsion of the patellar ligament from the tibial tubercle. The quadriceps muscle inserts into the patella by way of the quadriceps tendon and then into the tibial tuberosity by way of the patellar tendon. To keep away from this complication, an extensile publicity is required to loosen up the extensor mechanism and permit secure eversion of the patella. Note that the medial and lateral patellar retinaculae originate proximally from the tendinous fibers of the vastus medialis and lateralis muscle tissue, respectively. Tibial tubercle osteotomy is preferred as a end result of it has a decrease incidence of extensor lag and quadriceps weakness compared to a V-Y quadriceps turndown. A tourniquet is sited across the upper thigh, and the leg is exsanguinated before inflation. A clamp is positioned laterally to stabilize the decrease leg when the knee is flexed. A sandbag is positioned distal to the foot to forestall the decrease leg from sliding throughout surgery. Approach A medial parapatellar method is used whenever attainable, as a outcome of extensile exposures are most simply included proximally (V-Y quadriceps turndown) and distally (tibial tubercle osteotomy). The radiographs are particularly inspected for tibial osteopenia and osteolysis, both of which are relative contraindications for tibial tubercle osteotomy. First the suprapatellar pouch, with the lateral gutter, is free of underlying adhesions. The 6-cm medial, vertical limb of the osteotomy is tapered distally to prevent a stress riser. The 2-cm horizontal limb proximal to the insertion of the patellar tendon resists proximal migration of the osteotomized segment. Sequential osteotomes are used to transect the medial tibial crest and separate the osteotomized section from the tibia. The lateral cortex is transected through the osteotomy, however the lateral periosteum and delicate tissues are left hooked up to the elevated segment to act as a "hinge," permitting eversion of the extensor mechanism. The medial cortex is perforated with a drill, and the drill is passed through the lateral cortex to create corresponding perforations in the lateral cortex that can allow the osteoperiosteal phase to be "hinged" around the lateral gentle tissue attachments. The proximal osteotomy minimize is perforated, and sequential osteotomes are used to elevate the osteotomy. The most proximal wire is passed via the osteotomized phase and through a drilled hole within the medial tibial cortex. The wires are twisted until tight, reduce, and angled forty five levels posteromedially to stop delicate tissue irritation. The most proximal wire is handed via the osteotomized segment to forestall proximal migration; the 2 distal wires are handed across the osteotomy phase. The screws are handed posteromedially and posterolaterally around the tibial component using the triangular cross section of the proximal tibia. Medial launch, meticulous lateral gutter launch, and excision of pseudocapsule earlier than tibial tubercle osteotomy. Reattachment of osteotomy Anatomic fixation of the osteotomized section is critical to guarantee union of the osteotomy. At least one wire is handed by way of the osteotomy fragment to forestall proximal migration. At 2-year follow-up, the imply postoperative vary of movement was 94 degrees, with a 1. Three tibial shaft fractures and two avulsions of the tibial tubercle have been reported in this series, however no non-unions. At a median follow-up of 30 months, the mean postoperative range of movement was 107 degrees, with a four. One fracture of the tibia, no tibial avulsions, and two non-unions of the osteotomy have been reported on this series. Barrack1 reported a considerably decrease incidence of extensor lag following tibial tubercle osteotomy when in comparability with V-Y quadriceps turndown, although outcome scores were related for each groups at the 4-year follow-up. Biomechanical research present that although reattachment of an osteotomy with screws has higher fixation strength than cerclage wires, placement of screws round revision tibial part stems is troublesome. High rates of fixation failure with tibial tubercle osteotomy most likely are because of using small (3 cm) osteoperiosteal fragments and failure to preserve lateral soft tissue attachments in continuity with the osteotomized segment. Quadriceps snip is used mostly, adopted by tibial tubercle osteotomy or V-Y quadriceps turndown. Although it could be potential to carry out a prosthetic implantation with out utilizing an extensile publicity in the ankylosed knee, quadriceps contracture can limit extensor mechanism tour, resulting in poor postoperative flexion. V-Y quadricepsplasty could additionally be performed after prosthetic insertion to improve flexion. Although a straight, midline anterior incision is preferred, because the vascular supply to this skin is primarily from the medial aspect, probably the most lateral useable incision is chosen. A medial parapatellar arthrotomy is then made at the junction of the medial and central thirds of the quadriceps tendon. Subperiosteal dissection of the tibia is then extended from the tibial tubercle to the posteromedial corner, together with launch to the semimembranous insertion. A suprapatellar pouch, in addition to the medial and lateral gutters, is then reestablished, all adhesions are released, and a radical synovectomy is carried out.
Order rulide 150 mg free shipping
Standard skin closure is carried out treatment jellyfish sting discount rulide 150 mg free shipping, and the arm is splinted or casted at ninety levels of elbow flexion medicine z pack purchase 150 mg rulide mastercard. Fluoroscopic picture showing two pins spanning the fracture fragment for rotational stability. This would involve sutures placed directly within the tendinous tissue and secured to the periosteum adjoining to the bed from which the epicondyle was avulsed. This technique is best within the first 24 hours after the harm, before much muscle spasm happens. Elbow movement is inspired as soon as possible after surgical procedure to decrease postoperative stiffness. Some authors recommend a detachable brace stopping valgus stress but allowing full flexion and extension for 4 weeks. At 8 weeks noncontact sports activities were allowed, and return to full activity was attainable at 12 weeks after surgical procedure. Surgical treatment of displaced medial epicondyle fractures in adolescent athletes. Long-term outcomes of therapy of fractures of the medial humeral epicondyle in youngsters. Operative remedy of displaced medial epicondyle fractures in youngsters and adolescents. One patient had a loss of 5 levels of hyperextension, however all different patients had recovery of full range of motion. Preoperative Planning During preoperative planning, the surgeon should contemplate the the reason why an open procedure is necessary. Other components for consideration embrace the pin measurement for sustaining the discount as soon as the fracture is lowered. The coronoid fossa is situated anteriorly and the olecranon fossa is positioned posteriorly. The neurovascular anatomy to think about for an open discount contains: the ulnar nerve passes behind the medial epicondyle. The radial nerve programs from posterior to anterior simply above the olecranon fossa. The surgeon ought to make certain that the fluoroscope could be moved easily into and out of the operative subject to assist with pinning of the fracture. This could represent buttonholing of the proximal fragment via the periosteum and brachialis muscle, making closed discount tough. Approach the first issue to think about in determining the method is the direction of displacement of the distal fragment. In general, a transverse anterior incision via the antecubital fossa is essentially the most helpful and beauty. If more visualization is needed, this incision can be prolonged medially or laterally based on displacement, however this is hardly ever needed. Extension of the incision on the alternative side of the displacement of the distal fragment allows for removing of soppy tissue obstacles to reduction. An incapability to scale back the fracture might indicate that the proximal fragment has buttonholed through the brachialis muscle. Some surgeons have advocated a posterior method for severely comminuted fractures. Some newer articles have been printed finding no significant enhance in complication charges with delayed therapy. It is at this point that the neurovascular bundle must be located, if it has not yet been recognized. This normally includes dissecting across the anterior facet of the metaphyseal spike. Defining the outline of the distal fragment can be probably the most challenging aspect of the procedure. Reduction is obtained by reaching into the fracture web site with a hemostat and getting hold of the reduce edge of the periosteum. This cut edge is extended with scissors to improve the scale of the buttonhole and helps to unlock the distal fragment. The distal fragment is then brought anteriorly and decreased to the shaft fragment, which is maneuvered back via the buttonhole into its resting position posterior to the brachialis muscle. Alternatively, the surgeon can maintain his or her thumb on the proximal fragment and push downward whereas an assistant applies traction to the forearm with the elbow flexed at 90 degrees. Pinning Once a reduction has been obtained, the fracture is fixed with clean Kirschner wires. Sagittal view of fracture with proximal fragment proven buttonholing although muscle and periosteum. Alternatively, a cross-pinning strategy can be used with medial and lateral entry pins. Ideally, both the medial and lateral pins ought to cross proximal to the fracture web site. The surgeon must be positive to have interaction each the medial and lateral columns of the distal fragment. The surgeon ought to broaden the buttonhole via the periosteum for better visualization. Pins must be maximally separated at the fracture website if three lateral pins are used. If medial and lateral pins are used, the surgeon ought to interact the medial and lateral columns of the distal fragment. A strip of Xeroform dressing may be wrapped across the pins, adopted by fluff dressings. Often a long-arm solid could be placed safely the subsequent day, with the arm flexed about eighty levels. This cast could be maintained until the pins are eliminated 3 or four weeks after surgery. The patient can then be placed back right into a sling and began on gentle range-of-motion workouts out of the sling for another 2 weeks. Families must be advised about this longer period of elbow stiffness in the instant postoperative period. A 2001 examine of 862 supracondylar fractures treated with open discount discovered 55% excellent outcomes, 24% good outcomes, 9% honest outcomes, and 12% poor outcomes 5. Iatrogenic neurovascular injury Identification of neurovascular constructions is essential. Compartment syndrome the child ought to be kept in a single day for observation and the surgeon should be sure that serial neurovascular examinations are carried out.
Rulide 150 mg online buy cheap
Total knee arthroplasty after spontaneous osseous ankylosis and takedown of formal knee fusion symptoms neck pain cheap rulide 150 mg with mastercard. Arthrodesis of the knee after an contaminated total knee arthroplasty utilizing the Ilizarov method medications similar to gabapentin rulide 150mg discount with mastercard. Failed total knee arthroplasty handled by arthrodesis of the knee utilizing the Ace-Fischer equipment. Rud and Jensen11 examined 23 knee athrodesis patients and found that 18 had returned to work. Most patients ought to anticipate to have issue with stairs, rugs, and ladders,12 and sufferers who carried out strenuous work before the arthrodesis not often resume that strenuous work postoperatively. Rand et al10 reported that seven sufferers with knee arthrodeses could stroll one to three blocks and 9 profitable knee arthrodesis patients have been able to walk greater than six blocks. Compared with the alternative-above-the-knee amputation-knee fusion presents a stable, painless, and uninfected limb for weight bearing. The finest way to obtain one of the best outcomes for these sufferers with tough issues is to be thorough in the preoperative discussions regarding what knee arthrodesis can obtain for them. The clinician ought to determine whether the affected person has another complaints of ache beyond the forearm shaft region (eg, wrist or elbow tenderness). Any perceived deformity or ache to palpation should set off devoted radiographs of the problematic region. Any wound, no matter how small or seemingly superficial, ought to be carefully evaluated. Persistent bleeding or oozing from a small suspicious wound should be considered an open fracture until proven otherwise. The environment of the injury has special significance for open fracture management. For occasion, farm-related injuries may alter the remedy regimen for the affected person. Multiple trauma or high-energy trauma situations dictate that a screening orthopaedic examination be performed to assist rule out injuries to the opposite extremities in addition to the backbone. Brachial, radial, and ulnar pulses must be palpated and distal capillary refill ought to be assessed. Sensory examination should embrace, at minimum, mild touch sensation testing (or pin prick testing if necessary) of the autonomous zones of the radial, ulnar, and median nerves. Older kids might have the ability to comply with formal two-point discrimination testing. Anatomically the shaft of the radius extends from essentially the most proximal side of the tubercle of Lister (which approximates the distal metaphyseal�diaphyseal junction) to the proximal base of the bicipital tuberosity. Classically, forearm shaft fractures are divided into distal third (pronator quadratus region), central third (pronator teres region), and proximal third (biceps and supinator region). Forward falls tend to involve a pronated forearm and backward falls a supinated forearm. Single-bone forearm shaft fractures ought to raise significant suspicion regarding the presence of a Galeazzi or Monteggiatype damage (see Chap. Mechanisms of harm that contain little rotational force lead to forearm fractures at nearly the identical levels, while greater rotational drive results in fractures at quite totally different levels. Spontaneous correction and improvement of malaligned shaft fractures are considered to occur in younger kids by way of three mechanisms: Adjacent physes produce "straight bone" via regular growth. It has been said that you simply need only a thumb to test the motor operate of all three major nerves: radial nerve extensor pollicis longus, ulnar nerve adductor pollicis, median nerve opponens pollicis. Peripheral nerves in the fractured extremity are assessed with the "rock-paper-scissors" method. The radial nerve (really the posterior interosseous nerve within the forearm) is examined with "paper"-extension of the fingers and wrist well above a zero-degree wrist position. There is a threat of iatrogenic injury throughout surgical publicity of the proximal radial shaft. The ulnar nerve is tested with "scissors"-adducted thumb, kidnapped fingers, and flexor digitorum profundus function to ring and pinky. This is the most common iatrogenic nerve harm after inside fixation of forearm shaft fractures. The median is probably the most commonly injured nerve after closed or open forearm shaft fractures. Flexion of the distal interphalangeal of the index finger and the interphalangeal of the thumb herald flexor digitorum profundus and flexor pollicis longus function of these digits. Isolated palsy has been reported secondary to constrictive dressings and after proximal ulna fracture. Radius Ulna Level: Fracture stage has bearing on nonoperative versus operative determination making. Distal third Middle third Proximal third Pattern: Fracture pattern has bearing on nonoperative versus operative decision making. Bow (also often identified as plastic deformation) Greenstick Complete Comminuted respect should be paid to the extent of the fractures when choosing a relatively neutral, pronated, or supinated forearm place. Initial above-elbow forged immobilization is the rule for all forearm shaft fractures, as this appropriately controls pronation�supination in addition to obeying the orthopaedic maxim of immobilizing the joints above and beneath the fracture. An further good thing about above-elbow immobilization relates to the activity limitation it imposes; in some cases this will enhance the possibilities of sustaining a passable discount in an in any other case very active buyer. Successful nonoperative therapy requires an eclectic mix of anatomic data, skillful utility of reduction methods, appreciation for transforming potential, and respect for the character of the gentle tissue envelope. Davis and Green reported a 10% lack of discount price with greenstick fractures and a 25% rate with full fractures. Apex volar greenstick fractures are thought-about to symbolize supination injuries that require a relative degree of pronation to impact reduction. Apex dorsal greenstick fractures are considered to be pronation accidents that require supination to aid discount. Classic finger-trap and traction discount techniques are most likely finest reserved for complete both-bone fracture patterns. When coping with full both-bone shaft fractures, Flexible intramedullary nail treatment of pediatric forearm shaft fractures focuses predominantly on displaced full fractures, many of which may have minor comminution (butterfly fragments normally lower than 25% of a shaft diameter). When full fractures occur in youngsters youthful than about 8 to 10 years of age with angulation of a minimum of 20 degrees in the distal third, 15 levels in the central third, or 10 levels in the proximal third, risk�benefit discussions are appropriate concerning additional efforts at fracture discount and possible inner fixation. Complete forearm shaft fractures in children older than 8 to 10 years of age ought to be evaluated very critically with the intention to accept not extra than 10 levels of angulation at any degree. Preoperative Planning Rotational alignment of the radius and ulna must be assessed and estimated using the rules mentioned in the Anatomy part. Concern is increased if higher than 45 degrees of rotational malalignment is judged to be present. Measurement of the narrowest canal diameter of the radius (usually midshaft) and ulna (usually distal third) will help in the number of appropriately sized intramedullary nails. Implants 2 mm in diameter or smaller are commonly used, and the same-sized nail is used in every bone. Significant comminution may lead the surgeon to select plate fixation over intramedullary fixation for one or both bones.
Rulide 150 mg buy cheap on line
Tenderness to palpation should be assessed and localized specifically as it can tremendously direct the diagnosis of associated accidents treatment junctional tachycardia rulide 150 mg buy online. Tenderness to palpation alongside the joint line symptoms rabies rulide 150mg safe, notably the posterior side of the joint line, ought to alert the clinician to the potential of a meniscal tear. Pain or palpable popping with provocative maneuvers, similar to McMurray, Apley compression, or duck stroll, will help to affirm this finding. Pain alongside the course of or at the femoral or tibial insertion points for the collateral ligaments should alert the clinician to the risk of a collateral ligament tear. Tenderness along the medial retinaculum or the course of the medial patellofemoral ligament can point out an acute patellar dislocation that decreased spontaneously. Ligamentous analysis should embody the anterior and posterior cruciate ligaments, the medial and lateral collateral ligaments, and the posterolateral nook. Skeletally immature athletes have a larger degree of physiologic laxity than grownup athletes, and as such a comparison should all the time be made to the unhurt knee. In the patient who voluntarily or involuntarily guards against traditional Lachman testing, the prone Lachman could encourage leisure and provides a more dependable examination. Pivot shift testing may be carried out within the workplace however is normally not nicely tolerated by pediatric patients. It ought to be performed within the working room as part of the preoperative analysis of every patient. The posterior cruciate ligament must be evaluated using the posterior drawer check. The relative starting point should all the time be assessed first and compared to the contralateral side. Medial and lateral collateral ligament accidents are assessed by way of stress opening with valgus and varus stress at 0 and 30 degrees of knee flexion. In the pediatric affected person, opening with varus and valgus stress could be because of physeal accidents, and the clinician ought to all the time be vigilant for this. The posterolateral drawer and the exterior rotation recurvatum exams are additionally helpful for evaluating posterolateral nook injuries. Evaluation for patellar instability with apprehension testing ought to be carried out. Evaluation of quadriceps bulk and power is necessary for postoperative restoration. Special attention ought to be given to evaluate for physeal injuries in addition to other accidents on the differential analysis. Overall varus and valgus malalignment, if current clinically, ought to be evaluated with full-length, hip-to-ankle radiographs. This is in all probability going due to the increased vascularity of the meniscus, which is often interpreted as intrasubstance degeneration or a tear of the meniscus. For prepubescent sufferers with recurrent instability despite the above therapy, reconstruction is indicated. A tensioned gentle tissue graft in a bone tunnel across the physis can even induce a development disturbance. A number of reconstructive techniques have been used, together with physeal-sparing, partial transphyseal, and transphyseal strategies using varied grafts. In prepubescent patients with massive quantities of growth potential remaining, we perform a physeal-sparing, mixed intra-articular and extra-articular reconstruction utilizing autogenous iliotibial band. Recognizing that the physeal-sparing reconstruction described right here is nonanatomic, we counsel patients and families that revision reconstruction may be wanted if recurrent instability develops, but that this process might temporize for further progress such that the patient could then endure a more typical reconstruction with drill holes. The following standards have been shown to be related to profitable nonoperative therapy of partial tears8: Tears of less than 50% of the ligament Relative preservation of the posterolateral bundle Age lower than 14 years Normal or near-normal Lachman or pivot shift test Up to a 3rd of sufferers might require subsequent reconstruction and should be made aware of that risk on the onset of therapy. Successful treatment primarily based on the above criteria consists of: A hinged knee brace is worn for 12 weeks. Return to sports and energetic play is permitted at three months with the usage of a practical knee brace for 2 years for cutting and pivoting actions. Nonoperative management of complete tears in skeletally immature sufferers generally has a poor prognosis. In our experience, compliance with exercise modification and brace use and effectiveness limits the success of this treatment. Delay in surgical stabilization can result in further meniscal and chondral injury because of recurrent instability. Consideration should be given to using pediatric anesthesia companies, given the age of the affected person. Tanner staging ought to be confirmed at the time of surgical procedure after the induction of basic anesthesia. A full ligamentous knee examination, together with Lachman, pivot shift, varus and valgus stress, posterior drawer, and dial exams, must be performed and the findings in comparability with the contralateral facet to affirm the prognosis. Local anesthesia with sedation may not be reliable in this inhabitants and has the potential for a paradoxical effect of sedation. The affected person is placed supine on the working room desk and moved close to the operative side of the table such that the operative leg easily drapes over the edge of the table. A side post is placed two fingerbreadths above the flexed knee because it drapes over the side of the bed. Autograft is preferred, but delicate tissue allograft could be thought of based mostly on patient desire. Allograft would negate the necessity for hamstring harvest within the transphyseal reconstruction. Proximally, the iliotibial band is separated from subcutaneous tissue using a periosteal elevator underneath the skin of the lateral thigh. The iliotibial band is indifferent proximally underneath the pores and skin using a curved meniscotome or an open tendon stripper. Alternatively, a counter-incision can be made at the upper thigh to launch the tendon. A small groove is made within the anteromedial proximal tibial epiphysis underneath the intermeniscal ligament utilizing a curved rat-tail rasp to convey the tibial graft placement extra posterior. Arthroscopy Graft Fixation Diagnostic arthroscopy of the knee is performed by way of normal anterolateral viewing and anteromedial working portals. The over-the-top place on the femur and the overthe-front position underneath the intermeniscal ligament are recognized and cleared of extra tissue to permit passage of the graft. Minimal notchplasty is performed to keep away from iatrogenic damage to the perichondrial ring of the distal femoral physis, which could be very close to the over-the-top position. Fluoroscopic imaging is used to assess the location of the proximal tibial physis. A longitudinal incision is made within the periosteum distal to the proximal tibial physis. The anterior and posterior elements of the iliotibial band are recognized by way of a laterally based incision at the knee. A meniscotome or an open tendon stripper is then used to harvest the proximal aspect of the graft. The free proximal facet of the graft is tubularized and left connected distally to the tubercle of Gerdy.
150mg rulide cheap with mastercard
A prophylactic subcutaneous release of the anterior compartment is then performed through this incision symptoms electrolyte imbalance rulide 150 mg discount on line. Care ought to be taken to avoid shredding the umbilical tape symptoms 7 days pregnant cheap 150mg rulide amex, which can go away foreign materials behind. The Gigli saw is then tied to the umbilical tape to pass the noticed across the again of the tibia. Fluoroscopy is used to verify the completion of the osteotomy and alignment of the proximal and distal fragments with the exterior fixator. During the primary postoperative week, the patient learns to walk with crutches, 10 kilos, partial weight bearing. On the 8th day, the patient is taught to lengthen via the compression distraction mechanism at a price of 1 90-degree turn of the Allen wrench 4 instances a day. The patient is taught to place the Allen wrench into the first angulation screw and switch 90 levels within the path for angular correction. Secondary deformity (flexion or extension) may be corrected via the secondary hinges, translation screws (one 360-degree flip translates 1 mm), lengthening screws, and the rotation arc (one 90-degree flip corrects 1 diploma of rotation). The system can be safely removed after passage of at least 1 month per centimeter of lengthening and a minimum of about 3 months. Training and expertise with external fixation and deformity correction is at all times advised. All half-pins have to be positioned into protected zones of the leg to keep away from inadvertent neurovascular damage. No adjustments or corrections are made to the external fixator for the first 7 days. The correction phase begins with lengthening the leg by 7 to 8 mm at a price of 1 mm per day (0. The affected person is evaulated clinically and radiographically to follow correction of the mechanical axis. Scanograms can then be obtained to determine leg-length inequality, which can be corrected by lengthening with the fixator. Placing white adhesive tape with arrows onto the gadget helps sufferers keep in mind tips on how to turn the screws appropriately for angular, linear, and rotational correction. They can walk with crutches initially and progress to full weight bearing as the osteotomy heals. When radiographs show that the ostetotomy and distraction hole have healed, the exterior fixator is eliminated. Considerable torque is required to take away hydroxyapatite pins, and this have to be carried out in the operating room with adequate sedation and analgesia. Price et al5 reported on the therapy of 31 tibiae in 23 sufferers with dynamic exterior fixation. There was a mean correction of 20 levels, and no postoperative loss of correction occurred. Steel et al8 reported a 20% fee of neurologic problems in 46 tibial osteotomies. The neurologic problems are associated to the placement of the osteotomy, which should be done within the metaphysis to keep away from damaging the proximal tibial epiphysis. Deformity correction at this stage can stretch or compress the anterior tibial artery because of its proximity to the tibia at that degree. While arterial stretch or compression is extra frequent than laceration or edema in anterior compartment following correction, prophylactic fasciotomies of the anterior and lateral compartments are still indicated to lower the risk of neurovascular complications. Use of the Ilizarov methodology to correct decrease limb deformities in children and adolescents. With epiphysiodesis, progress of a longer extremity is inhibited by prematurely arresting a particular physis so that the remaining development of the shorter extremity might approximate or equalize limb lengths at maturity. The open epiphysiodesis technique was first described by Phemister in 193320 and modified by White in 1944. Useful knowledge in decision making embody: Body size from head to foot (to determine percentile of height) Length of the bones of the decrease extremity (to determine diploma and supply of discrepancies) Skeletal maturation age (to determine potential remaining growth), and the disease course that triggered the limb inequality (to decide the predictability of remaining growth) Proper affected person age for timing of the epiphysiodesis could also be decided by a quantity of strategies, together with the Green and Anderson methodology,10 the Mosley straight-line methodology,sixteen the "rule of thumb" technique,15 and the multiplier methodology. The aim of physeal stapling is to retard progress of a physis with staples till the specified correction is obtained, after which the staples can be eliminated, with physeal development resuming until maturity. The frequent peroneal nerve on the knee runs obliquely along the lateral side of the popliteal fossa, close to the medial border of the biceps femoris muscle and the lateral head of the gastrocnemius muscle, towards the top of the fibula. The nerve winds posteriorly around the neck of the proximal fibula and passes deep to the peroneus longus muscle, the place it divides into the superficial and deep peroneal nerves. Shapiro reported totally different patterns of growth inhibition that will cause shortening of a limb. After peripheral bony bar formation following a percutaneous epiphysiodesis, the central space of the physis (unoperated area) will spontaneously shut inside 6 to eight months. I even have not had a patient have this complication, however follow-up till skeletal maturity is suggested. By following development till maturity, this potential drawback could also be detected and a contralateral epiphysiodesis could forestall a limb-length discrepancy at maturity. A percutaneous epiphysiodesis can be used in combination with contralateral limb lengthening in patients with severe shortening. In main limb-length discrepancies, lengthening may not have the flexibility to right the complete discrepancy, and remaining small discrepancies of two to 5 cm may be more easily corrected by a contralateral percutaneous epiphysiodesis than by a secondary ipsilateral lengthening. After leg-lengthening procedures, development of the lengthened limb could additionally be retarded or occasionally stimulated. These subsequently kind bony bars that limit development, after which the central aspect of the physis closes spontaneously, leading to a complete epiphysio�diaphyseal fusion. Caution is required within the femur distally as a outcome of the epiphysis is slim on the central space of the physis. Posteriorly the neurovascular constructions are deeply positioned inside the condyles, and anteriorly the patella�femoral joint is shut. Therefore, I prefer the peripheral margin ablation technique as described here, by which the central space of the physis remains undisturbed. The percentile of top is then decided and used to plot limb-length predictive charts. The level of maturation, based mostly on the looks of secondary sexual traits and the Tanner scale. These measurements are plotted on progress charts to predict the discrepancy at maturity and to decide the age for epiphysiodesis. Blocks of differing thicknesses are positioned under the foot of the shorter limb until the pelvis is degree to determine the length discrepancy (expressed in centimeters). After length measurements of each limbs are obtained, the ratio of femur to tibial discrepancy of the normal to irregular limb is set. This may be achieved by different techniques and instruments, which include a curette, a drill, a burr, a reamer, and a round tube saw. I favor a curette because surgeon management is simple and the curette may be passed percutaneously. I have used varied devices, however drills and burrs are inclined to burn and sometimes grab tissue, and reamers and round saws require a bigger incision (really not percutaneous, nearly the scale of a typical open epiphysiodesis). A bony bridge needs to type only on the peripheral margins of the physis both medially and laterally to accomplish an epiphysiodesis.
Mallaguetta Pepper (Grains Of Paradise). Rulide.
- How does Grains Of Paradise work?
- Are there safety concerns?
- Dosing considerations for Grains Of Paradise.
- What is Grains Of Paradise?
- Use as a stimulant.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96660
Proven 150mg rulide
The plate should be parallel to the posterior trochanteric border to ensure correction of the flexion deformity symptoms 0f yeast infectiion in women purchase 150mg rulide. The second osteotomy is began at the parallel cut and directed distally in an indirect trend symptoms rheumatoid arthritis rulide 150 mg buy free shipping. The distal segment overlaps the proximal phase because of the delicate tissue constraints. This determines the amount of shortening required and the place of the third osteotomy. For sort 1b instances, an adjunct therapy could be performed by drilling a channel with a diameter of 3. The stability of the graft is examined by making an attempt to pull the graft from the osteotomy web site with a Kocher clamp. The crest is then resected using a noticed till the medial and lateral apophysis may be repaired with out excessive pressure. The femur is positioned in impartial abduction, and the conjoint abductor�quadriceps tendon is sutured directly into the cartilaginous higher trochanter with absorbable suture beneath some tension. A suction drain is used and is left in place till the draining stops (less than 10 cc per 24 hours), which can take several days. Prophylactic antibiotics are administered intravenously until the drain is removed. A spica forged is applied with the hip in full extension, impartial abduction, and impartial rotation. In the coronal plane, the apex of the osteotomy starts 2 cm above the joint and is inclined towards the triradiate cartilage medially. The proximal side of the incision is developed as described for the superhip procedure. The biceps femoris tendon should be Z-lengthened if knee flexion deformity is present or if the tibia is externally rotated on the femur. A lateral release of the capsule leaving the synovium intact is performed in all circumstances. A Grammont procedure4 is performed to medially transfer the patellar tendon if patellar maltracking is important. This procedure is finished by releasing the patellar tendon from proximal to distal and from lateral to medial, leaving intact a protracted sleeve of periosteum distally. The periosteal extension of the tendon is elevated with the tendon so that the indifferent tendon remains tethered distally. Grammont patellar tendon medialization is carried out by incising the medial and lateral borders of the patellar tendon previous the tibial tubercle. The patellar tendon is elevated off the tibial tubercle apophysis with an extension of periosteum that continues to be intact distally. The anterior and posterior margins of the fascia lata are recognized and dissected proximally. If the patella continues to be tethered laterally by the vastus lateralis muscle, its tendon is released from the lateral aspect of the patella and transferred centrally to the quadriceps tendon underneath minimal pressure. The lateral release is extended distally to the lateral facet of the patellar tendon. If a Grammont procedure4 is to be carried out, the incision is prolonged past the tibial tuberosity along the crest of the tibia so that the proximal periosteum is elevated as described above. The other tunnel is made subperiosteally, from anterior and proximal to posterior and distal, over the lateral intramuscular septum of the femur. A hole is made in the posterior knee joint capsule by inserting a curved clamp from the "over-the-top" place. The wire is inserted from the anteromedial side of the tibia and is directed to the middle of the tibial epiphysis. A suture passer is handed via the tibial epiphyseal tunnel and out the posterior capsule of the knee to exit laterally anterior to the septum. The fascia lata suture is pulled through the knee and the bony tunnel using the suture passer. To forestall loosening, the graft can be bolstered and retensioned after fixation by passing a nonabsorbable suture by way of bone at the point at which the graft loops over the intermuscular septum. Lateral collateral ligament and the distal side of the posterior intramuscular septum are recognized. The posterior limb of the fascia lata graft is handed underneath the lateral collateral ligament. Posterior limb is then handed through a subperiosteal tunnel beneath the lateral intermuscular septum. The graft enters the subperiosteal tunnel from the anterior aspect and heads distally towards the posterior knee joint capsule. The wire is directed toward the lateral femoral condyle and exits the tibial epiphysis on the midpoint of the ossification middle. This wire is overdrilled with the appropriate-size cannulated drill, depending on the graft measurement. Suture passer is inserted into the bony tunnel and retrieved on the posterior side of the knee with a curved clamp. Alternatively, as an alternative of a combined intra-articular and extraarticular restore, an isolated extraarticular reconstruction can be carried out. The graft is then tensioned with the limb in full extension, folded back onto itself, and secured with nonabsorbable suture. It is passed first underneath the patellar tendon after which through a medial capsular tunnel. The graft is then passed via a subperiosteal tunnel around the adductor magnus tendon. This extra-articular ligament is tensioned with the knee in 90 levels of flexion to forestall an extension contracture. To expose the medial side, the medial gentle tissue flap is mirrored to the midline. An anterior-to-posterior drill gap is made via the epiphysis, and the anterior limb of the fascia lata is handed from anterior to posterior, exiting near the midline posteriorly. Another drill gap that passes via the medial distal femoral epiphysis from anteromedial to posterolateral is made. The ligamentized fascia lata is pulled via the posterior capsule and into the medial femoral epiphyseal tunnel utilizing its leading suture. It is mounted in place with a biotenodesis absorbable screw (Arthrex) after tensioning in flexion. The posterior facet of three: Anterior limb of fascia lata passed beneath adductor magnus tendon If the patella has a hard and fast lateral subluxation or dislocation, a modified Langenski�ld patellar reconstruction is carried out earlier than the knee ligamentous reconstruction (intra-articular and extra-articular). Reverse MacIntosh (extra-articular posterior collateral ligament) process is carried out by passing the anterior limb of the fascia lata graft underneath the patellar tendon and through a window created within the medial joint capsule.
Rulide 150mg sale
The angular difference between the tibial shaft and a vertical line signifies the anteversion symptoms 6dpiui rulide 150 mg buy discount on-line. Excessive femoral anteversion is typically seen in neuromuscular circumstances and in developmental dysplasia of the hip and leads to medicine valley high school generic rulide 150mg amex extreme inner hip rotation and a corresponding lack of exterior hip rotation when tested in the inclined position. The tip of the larger trochanter is on the degree of the center of the femoral head. The neck�shaft angle at birth is often a hundred and fifty levels, lowering to a hundred thirty five degrees by skeletal maturity. Normal anteversion at start is forty five degrees, lowering to 10 degrees in boys and 15 levels in girls by 8 years of age. Both of those can be affected by neuromuscular conditions similar to cerebral palsy or myelomeningocele. Even so, with good neuromuscular perform, varusizing the femur could be well tolerated and can enhance the containment of the diseased femoral head. Contributing elements to the hip joint pathology might embody musculotendinous contractures, ligamentous laxity, and coexistent acetabular dysplasia. Adductor lengthening, psoas lengthening, open discount of the hip with capsulorrhaphy, and acetabuloplasty may need to be considered. Proximal femoral deformity can have an adverse effect on hip joint improvement and exacerbates or contributes to muscle imbalance concerning the hip. Hip flexion and adduction deformities may be recognized by asymmetries in femoral place or uneven pelvic position. An examination underneath anesthesia can guide choice making concerning concurrent tendon lengthening. The effect on leg length can be controlled by altering the amount of varusization and the dimensions of the wedge of bone eliminated (if any) relying on preoperative leg-length assessment. This permits ease of publicity posterior to the muscle stomach of the vastus lateralis. The prone position also permits correct control of femoral torsion corresponding to the susceptible physical examination for femoral anteversion by palpation, thereby bettering consistency of surgical realignment. The process involves inserting the chisel for the blade plate in the acceptable place within the femoral neck comparable to the quantity of varus to accomplish (eg, 20-degree varus correction corresponds to 70-degree chisel placement relative to the lateral femoral cortical surface: 90-degree blade plate minus 70 levels equals 20 levels varusization), finishing the osteotomy, and placing the 90-degree blade plate as detailed within the Techniques section. The amount of varusization can be decided based mostly on radiographs preoperatively or on intraoperative findings. The vastus lateralis is reflected from its proximal and posterior origins and elevated to expose the proximal femur subperiosteally. The fascia of the vastus lateralis is divided transversely at the higher trochanteric apophysis and posteriorly within the periosteum of the intertrochanteric space and longitudinally adjoining to the insertion on the linea aspera (in the susceptible place, up is posterior). The vastus lateralis is elevated subperiosteally, and Crego retractors are placed circumferentially at the intertrochanteric level. The entry point is just under the higher trochanteric apophysis if the patient is skeletally immature and thru the greater trochanter after maturity. The entry point is chosen to allow insertion of the guidewire and chisel with out violating the medial calcar. If preoperative planning indicated a 15-degree varusization goal, a 75-degree triangle can be used (see the Approach part above). Alternatively, dedication could be made based mostly on preoperative and desired postoperative alignment; for instance, the preoperative neck�shaft angle (150 degrees) minus the specified postoperative neck�shaft angle (120 degrees) equals 30 degrees of varusization. In this case, the guidewire would be placed at a 60-degree angle to the femoral shaft when utilizing the 90-degree plate. Intraoperative C-arm view exhibiting the guidewire at a 110-degree angle to the femoral shaft. The ideal lateral projection with femoral neck, femoral shaft, and guidewire coplanar improves accuracy and consistency. The chisel ought to be dislodged 5 to 10 mm before the osteotomy to allow for ease of later removing. Alternatively, a wedge of bone could be removed to accomplish a medial closing osteotomy. The entry point for the osteotomy noticed blade is determined by the implant (distance between the blade and the next angle in the plate for medialization). The beginning level for this osteotomy varies relying on the specified quantity of shortening of the extremity. A beginning level similar to the entry level for the primary osteotomy achieves full contact of the osteotomy after fixation. An entry point proximal (within the cut of the primary osteotomy) leads to much less shortening, but incomplete last apposition of the osteotomy surfaces. Alignment is checked after placement of the first screw each radiographically and by bodily examination. Correction of deformity by reducing the plate to the femoral shaft with a Verbrugge clamp. Hip joint pathology must not preclude repositioning of the femoral head inside the acetabulum in a functional position of the leg. Accurate realignment Prone positioning promotes correct control, correction, or each of femoral torsion. Final alignment relies upon solely on the angle of pin insertion and the selection of blade plate angle (in this case, 90 degrees). Apposition of the osteotomy surfaces themselves additionally is determined by the orientation of the osteotomy cuts. Knee immobilizers enhance comfort by stopping flexion-extension attributable to spasms of the hip flexors and hamstrings. Weight bearing can range from toe-touch to non-weight bearing for the primary three to 6 weeks. With poor bone quality, small bone measurement, small implant measurement, or poor compliance, a spica cast must be applied. Unrestricted vary of movement without external immobilization may be allowed (eg, most adults). A range-of-motion and strengthening program usually is instituted at three to four weeks postoperatively. Advancement to full weight bearing may be accomplished inside 6 to eight weeks of the process, depending on muscle power. The stability of the hip in youngsters: a radiological research of outcomes of muscle surgery in cerebral palsy. The severity of the deformity varies broadly, and this situation could be diagnosed in the prenatal period using ultrasound examination. The affected limb grows at an inhibited rate relying on the severity of the underlying deficiency.
150mg rulide generic visa
The upper extremities medicine and health cheap rulide 150 mg with mastercard, backbone treatment gastritis rulide 150mg cheap otc, and ft are at all times inspected to consider for possible generalized circumstances similar to arthrogryposis or neuromuscular situations. In the child of walking age, a delay of strolling could be the first indicator that the hip is dislocated. Dipping of the pelvis and shoulder (Trendelenburg gait), feminine profile (pelvic widening from the dislocation), and shortening of the thigh (Galeazzi sign) are traditional indicators of a dislocated hip within the older youngster. Additional indicators of Trendelenburg gait include side-toside waddling, indicating weak hip abductors, or the examiner may see lurching, indicating weak hip extensors. These are proximal compensations for a hip dislocation and the resulting insufficient muscle strength to help the pelvis. The Von Rosen view in abduction and inner rotation exhibits the power of the femoral head to scale back. Coronal part ultrasound imaging through essentially the most posterior aspect of the acetabulum. Preoperative Planning For the infant who has not achieved strolling age, an open discount with out associated femoral shortening or pelvic osteotomy is mostly adequate. With age and walking, the deformities in and around the hip turn out to be extra fastened and require a more aggressive surgical approach. Epidural or caudal regional anesthesia could additionally be useful to complement the overall anesthesia. An indwelling bladder catheter is used through the surgical procedure, since much of the surgery is intrapelvic. Generally, the earlier that therapy is initiated, the extra probably that much less invasive remedy shall be profitable and that a greater end result will outcome. By the time of skeletal maturity, as normal as possible acetabular anatomy must be restored. Positioning A radiolucent desk is utilized in case an intraoperative radiograph will be obtained. Approach Several variations of the medial approach to the hip joint have been described. For the older infant and baby an anterior approach to the hip joint allows more extensile publicity. The anterior method allows for an associated pelvic osteotomy through the same incision. This toddler is comfortable within the harness; hips and knees are flexed with abduction offered by gravity, not from the lateral straps. The anterior hip and lateral thigh incisions are generally parallel when the hip is flexed about 30 degrees. This is the deep fascia, which may then be additional uncovered distally by utilizing a sponge on the fascia. If femoral shortening is anticipated, a separate direct lateral approach to the proximal femur is used. Both exposures must be completed before osteotomies are carried out due to elevated bleeding from the bone. The fascia of the tensor muscle is entered slightly lateral to the fatty interval between the two muscle tissue. Army-Navy retractors are used to separate the tensor and sartorius muscular tissues until the rectus femoris muscle is identified. This dissection is sustained proximally and the prow of the pelvis is exposed between the anterior superior and anterior inferior iliac spines. The iliac crest apophysis is divided exactly within the middle with a single cut utilizing a no. Laparotomy sponges are used to assist dissect deep close to the sciatic notch and to pack the surgical site for hemostasis. Perforating vessels into the iliac bone on the inside desk are consistently present and require bone wax for hemostasis. Smooth Lane retractors are used to additional dissect the sciatic notch both medially and laterally. By opening the medial periosteum on the degree of the pubis, the iliopsoas tendon is identified, which lies deep on the iliacus muscle. The tendon is adopted distally so that the interval between the iliacus muscle and the rectus femoris muscle is separated extra deeply. The iliopsoas tendon is brought into the superficial surgical website with a right-angled clamp and divided at the stage of the iliopectineal groove on the pubis. The external indirect muscle has been detached off the iliac crest apophysis, which is being divided by a no. The iliopsoas tendon is identified, dissected distally, and divided on the iliopectineal eminence. Deep muscles of the iliacus, rectus femoris, and gluteus medius are mirrored off the hip capsule. The capsule should be separated from any false acetabulum on the lateral iliac wall. The reflected and straight heads of the rectus femoris muscle are recognized and divided. With a Kocher clamp, grasp the proximal side of the reflected head of the rectus femoris tendon to additional expose the capsule. The capsule have to be detached from the false acetabulum if present and exposed superior and posterior. It is crucial to visualize the entire acetabulum and the transverse acetabular ligament. The ligamentum teres is removed with Mayo or cartilage scissors at its deep acetabular attachment. Under direct vision, a pituitary rongeur is used to remove the pulvinar tissue that lies within the acetabulum. After any associated femoral and acetabular osteotomies are carried out, the capsule is advanced medially. For youngsters over 2�3 years of age, particularly if the reduction is tight or unstable, a femoral shortening osteotomy is performed earlier than the capsule is closed. An adductor longus and gracilis tenotomy is usually not needed but could be included if these muscle tissue really feel excessively tight. The iliac crest apophysis is reapproximated with heavy suture and the external oblique muscle is reattached. A one-and-a-half spica forged is utilized with the hips in a secure "human" position with no more than 30 levels of flexion and abduction. The anterior edge of the gluteus medius muscle is recognized where it attaches to the larger trochanter. The vastus lateralis muscle should be divided off the posterior intermuscular septum so that the muscle innervation is left completely intact. Stiff Steinmann pins are inserted within the proximal and distal femur to be positive that a correct quantity of femoral rotation is supplied.