Solian
"Purchase 50mg solian mastercard, medicine 2355".
C. Jared, M.B.A., M.B.B.S., M.H.S.
Deputy Director, Tulane University School of Medicine
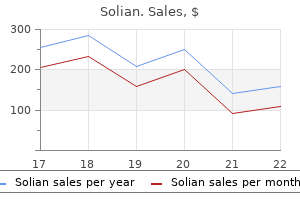
Culling Approximately 519 bison were captured at the Stephens Creek facility in the northern management area of Yellowstone National Park during January 14 through February 5 medications prolonged qt purchase solian 50mg otc, 2015 medicine you can take while pregnant generic solian 50 mg mastercard. Many bison had either moved beyond the capture facility or were already outside the park on days when captures occurred (Table 3) treatment xanthelasma eyelid cheap solian 100 mg on-line. Also 7 medications emts can give buy 100mg solian otc, many of the bison north of Stephens Creek had already returned to the park after being engaged by hunters close to the boundary. Seventy bison were harvested in the northern management area by January 22 and 145 bison were harvested by February 5. A total of 507 bison were shipped to processing facilities, including 347 by the Salish-Kootenai tribes, 138 by the InterTribal Buffalo Council, and 22 by the Eastern Shoshone tribe. Specific shipping dates were January 20-23, 26-28, and 30-31; and February 2-5, 11, and 18-20. All bison consigned to processing were shipped within two days after testing for brucellosis exposure. Seven bison were transferred to the Animal and Plant Health Inspection Service for fertility control research. Four bison died during confinement (starvation; unknown cause) or processing (broken leg; capture myopathy), and one bison was released from the facility. Numbers of bison observed north of the Stephens Creek capture facility or outside Yellowstone National Park in the northern management area of Montana during winter of 20142015 by personnel from the National Park Service. Capture operations occurred over three weeks between January 14 and February 5, 2015 (indicated by bold font). Date December 4 December 11 December 15 December 31 January 5 January 9 January 12 January 14 January 20 January 23 January 27 January 28 January 30 February 2 February 4 February 9 February 11 February 18 March 3 March 9 March 20 April 16 Stephens Creek to Park Boundary 0 0 0 0 0 78 17 105 53 25 50 20 37 25 0 0 0 1 0 0 2 2 North of Park Boundary 0 0 0 0 11 39 113 24 2 0 1 0 2 77 1 1 0 0 1 1 1 1 Eagle Creek Management Area 4 0 0 0 0 0 7 0 21 0 11 11 10 0 0 0 3 0 0 0 0 0 Total 4 0 0 0 11 117 137 129 76 25 62 31 49 102 1 1 3 1 1 1 3 3 Hazing In the northern management area, one hazing operation occurred on January 23, 2015 to remove 70 mixed bison from a private hayfield. In the western management area, operations began on March 27, 2015 due to bison moving into Zone 3, with 31 separate operations occurring over the following 80 days. Also, a hazing event occurred on October 26, 2015 due to bison moving into Zone 3. A spring haze-back operation to bring bison from the Gardiner basin back into the park was not necessary due to the mild winter weather and return of most bison on their own prior to May 1. The spring haze-back of bison from the Hebgen basin into Yellowstone National Park began on May 12. The number of bison counted by Montana Department of Livestock personnel outside Yellowstone National Park when hazing events occurred is provided in Appendix E. Given a high count of nearly 750 bison observed at the park boundary or beyond in early May, only about 400 bison were hazed back into the park, with little evidence of bison being hazed multiple times to get them to move on eastward toward the interior park ranges. On June 3, about 50 to 70 bison moved back into the park without being hazed and few bison remained outside the park after that time. Brucellosis Testing and Vaccination Serum from 481 bison captured at the Stephens Creek facility was tested for brucellosis exposure. Positive test results were obtained for 22 of 33 (67%) adult males, 23 of 80 (29%) yearling males, 4 of 58 (7%) male calves, 112 of 192 (58%) adult females, 25 of 67 (37%) yearling females, and 2 of 51 (4%) female calves. Cattle 200/4 320/10 22/1 11/1 55/4 Class Pairs/Bulls Pairs/Bulls Pairs/Bulls Pairs/Bulls Pairs/Bulls Date out October 17 November 3 On October 23, 2014, a three year-old cow was tested as part of 349 animals moving from the Park County Designated Surveillance Area to Carbon County. The cow was classified as a reactor on a serological test and later cultured Brucella positive. The reactor cow tested negative in 2013 prior to returning to Carbon County from the Park County Designated Surveillance Area. This cow was not pregnant; therefore, posed very little risk to herds adjacent in Carbon County. Four adjacent herds (approximately 500 head) were identified in Park County and required to test for brucellosis. An additional four adjacent herds (approximately 500 head) were required to test in Carbon County. The reactor herd completed their entire herd test in late November of 2014 with no additional suspects or reactors.
A fourth treatment bulging disc buy solian 50 mg otc, "undetermined" category consists of adult cases in which a food or wound source cannot be identified medicine for stomach pain discount solian 50 mg with visa. It has been suggested that some cases of botulism assigned to this category might result from intestinal colonization in adults medicine cabinet cheap 50mg solian mastercard, with in vivo production of toxin treatment by lanshin 100 mg solian free shipping. The medical literature suggests the existence of an adult form of botulism similar to infant botulism. In these cases, patients have had surgical alterations of the gastrointestinal tract and/or antibiotic therapy. It is proposed that these procedures may have altered the normal bacterial population of the gut and allowed C. Antimicrobial therapy is not recommended, due to concerns about increased toxin release as a result of cell lysis. Mortality: the mortality rate is high if treatment is not immediately administered. Onset: Adult: Usually 18 to 36 hours after ingesting food containing the toxin, although times have varied from 4 hours to 8 days. Symptoms: Adult: Initial symptoms may include double vision, blurred vision, drooping eyelids, slurred speech, difficulty swallowing, dry mouth, and muscle weakness. If the disease is not treated, symptoms may progress to paralysis of the arms, legs, trunk, and respiratory muscles. Early signs of intoxication consist of marked lassitude, weakness and vertigo, usually followed by double vision and progressive difficulty in speaking and swallowing. Difficulty in breathing, weakness of other muscles, abdominal distention, and constipation may also be common symptoms Infant: Constipation after a period of normal development is often the first sign of infant botulism. This is followed by flat facial expression; poor feeding (weak sucking); weak cry; decreased movement; trouble swallowing, with excessive drooling; muscle weakness; and breathing problems. Duration: Patients with severe cases that involve paralysis of the respiratory muscles may need mechanical ventilation and intensive care for weeks or months. Pathway: Clinical presentation develops after a person ingests the pre-formed toxin, or if the organisms grow in the intestines or in wounds, followed by toxin release. The ingested botulinum toxin (an endopeptidase enzyme) blocks peripheral cholinergic neurotransmission at the neuromuscular junction and cholinergic autonomic nervous system. The toxin acts by binding presynaptically to high-affinity recognition sites on the cholinergic nerve terminals and decreasing the release of acetylcholine, causing a neuromuscular blocking effect. The toxin is synthesized as a relatively inactive single-chain polypeptide with a molecular weight of ~150 kDa. It becomes an active toxin by selective proteolytic cleavage to yield the heavy and light chains that are linked by a single disulphide bond and non-covalent interactions. Frequency As noted, the incidence of the disease is low, but the mortality rate is high, if the disease is not treated immediately and properly. Source: National Botulism Surveillance, Centers for Disease Control and Prevention 4. Sources General info: the types of foods involved in botulism vary according to food preservation and cooking practices. Any food conducive to outgrowth and toxin production can be associated with botulism. This can occur when food processing allows spore survival and the food is not subsequently heated before consumption, to eliminate any live cells. Salt concentration from 4% to 5% is needed for inhibition of its spores (especially regarding type E), with a 5% concentration completely inhibiting their growth. Salt concentrations slightly lower than those providing inhibition tend to extend spore outgrowth time at low temperatures. A variety of foods, such as canned corn, peppers, green beans, soups, beets, asparagus, mushrooms, ripe olives, spinach, tuna fish, chicken and chicken livers, liver pate, luncheon meats, ham, sausage, stuffed eggplant, lobster, and smoked and salted fish have been associated with botulinum toxin. Infant botulism: Of the various potential environmental sources, such as soil, cistern water, dust, and foods, honey is the one dietary reservoir of C.
Diagnosis and Treatment Taeniasis: Diagnosis is difficult because the disease is usually asymptomatic symptoms zenkers diverticulum cheap solian 50 mg with amex. Detection often occurs when the patient sees proglottids in stool or undergarments in treatment 2 solian 50 mg without prescription. Traditionally a stool specimen is examined microscopically for characteristic Taenia eggs; however medications held for dialysis trusted solian 50mg, this test is not reliable symptoms diverticulitis cheap solian 50mg with amex. The tapeworm species can sometimes be determined by examination of expelled proglottids and/or the scolex. Molecular sequencing, where available, should be used to determine the exact species. Cysticercosis: Symptoms usually occur a long time after infection, leading to difficulty relating symptoms to the cause; because the disease is uncommon in the U. Computed tomography and magnetic resonance imaging are needed to identify the number, location, size, and other important characteristics of cysticerci in the brain. Less expensive serological techniques are constantly improving and may be used to confirm diagnosis and track the course of disease. Seizures, inflammation, and hydrocephalus must first be stabilized before considering treatment for the parasite. Treating cysticerci in the brain with anthelmintic drugs may activate a severe immune response, causing excessive inflammation; therefore, antiinflammatory and anthelmintic drugs are used judicially to facilitate removal of cysts. Shunts may be inserted to relieve intracranial pressure, and open or endoscopic surgery may be used to remove cysticerci in accessible locations. Recovered larvae should be identified for epidemiological reasons, because other tapeworm species also may cause cysticercosis. Food Analysis Regulatory authorities inspect pork and beef carcasses for "measled" meat by feeling and visually examining susceptible muscles for cysticerci. Examples of Outbreaks Taeniasis and cysticercosis are endemic in much of the world. In 1978, there was a large cysticercosis outbreak in West New Guinea after infected pigs were introduced into that country. The disease was recognized when there was an epidemic of burn victims who sustained their injuries during neurocysticercosis induced seizures that occurred as they slept near fireplaces. In 1990, a neurocysticercosis outbreak occurred in an Orthodox Jewish community, in New York City, that did not eat pork. The source of infection was thought to be recently immigrated housekeepers infected with pork tapeworms. Organisms For Consumers: A Snapshot Larvae of some nematodes (roundworms) in the family anisakidae can infect humans who eat raw or undercooked fish or cephalopods (marine mollusks, such as squid, octopus, and cuttlefish). These worms include: Anisakis simplex complex (herring worm) Pseudoterranova (Phocanema, Terranova) decipiens complex (cod or seal worm) Anisakis physeteris Contracaecum species A. These two species are now known to be complexes of multiple species that are distinguishable only by genetic analysis. Disease the name of the disease caused by these worms is anisakiasis or anisakidosis. Onset: Symptoms usually occur within 24 hours after consumption of affected raw or undercooked fish, but may be delayed by as long as 2 weeks. These worms are common in fish and squid, cuttlefish, and octopus, but proper cooking (described below) inactivates them. If you eat them alive in raw or undercooked fish, they can infect your stomach or intestine. If a worm burrows into the wall of the stomach or intestine, it can cause stomach or abdominal pain, nausea, vomiting, and diarrhea, from mild to severe. The worm generally is found and removed with an instrument called an endoscope; if done early, the symptoms usually go away immediately. Symptoms / complications: Non-invasive anisakiasis is often asymptomatic or sometimes is diagnosed when the affected person feels a tingling sensation in the throat and coughs up or manually extracts a nematode.
Given the risk of progression among high-risk patients is higher than any other group medicine identification cheap solian 50 mg fast delivery, the Panel felt a more intensive cystoscopic surveillance regimen was warranted medicine engineering 50 mg solian with amex. Panel consensus and historic precedence support surveillance cystoscopy and urinary cytology every three months for two years medicine man aurora purchase 100 mg solian fast delivery, then every six months for years three and four treatment dynamics florham park effective solian 100 mg, and then annually thereafter. As with intermediate-risk disease, there is an urgent need for studies to determine if less stringent follow up regimens can be employed without significantly affecting oncologic outcomes in these patients. As the risk of recurrence decreases and the time to recurrences increases beyond five years, a decision to decrease the frequency of cystoscopy or stop routine follow up cystoscopy after five years should only be made after a shared decision-making conversation with the patient. For an intermediate- or high-risk patient, a clinician should consider performing surveillance upper tract imaging at one to two year intervals. Retrospective cohort studies have suggested, however, that in a "higher-" risk cohort of patients, including those with higher-grade, multiple recurrences, or stage T1 disease, the subsequent rate of upper tract recurrence is as high as 10%69,186 of known low-grade Ta disease in which the size of the tumor was small (typically defined at less than 0. This has the potential to spare a patient the risks associated with anesthesia required for a more invasive resection in an operating room setting. For highly selected patients, clinicians may opt for watchful waiting or conservative management in those patients for whom the risks of fulguration may outweigh the risks of disease progression. This might include those cases where in-office fulguration is not readily available or patients who required ongoing anti-coagulation. A fulguration approach should be restricted to those patients in whom the lesion is papillary in appearance, rather than sessile or flat, and is no more than 1 cm in size. Furthermore, patients in whom a urinary cytology is suspicious for urothelial carcinoma are at higher risk for harboring occult high-grade disease and warrant pathologic evaluation of any visible lesion. Upper tract imaging to assess occult disease also may be considered in patients who develop repeated recurrences of small papillary lesions in the bladder. For an intermediate-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent cystoscopy with cytology every 3-6 months for 2 years, then 6-12 months for years 3 and 4, and then annually thereafter. The risk of progression, however, among these patients is higher, and in the absence of data to demonstrate otherwise, the Panel felt a slightly more intensive cystoscopic surveillance regimen was warranted. Panel consensus and historic precedence support surveillance cystoscopy and urinary cytology every three to six months for two years, then every six to twelve months for years three and four, and then annually thereafter. As research continues in this space, we are likely to see an increase in the number of available treatment options for such patients. Wider acceptance of intracorporeal urinary diversion in the urologic community could potentially have similar effects. As such, these recurrences, which are often high-stage and/or high-grade, are potentially life threatening. Whether routine imaging in asymptomatic patients is likely to diagnose such recurrences in a manner that actually improves oncologic outcomes or therapeutic options is controversial. Although many different salvage intravesical therapies have been evaluated, these studies are generally limited by small patient numbers, modest improvements in recurrencefree survival with respective intravesical agent(s), and no significant effects on progression or survival. These limitations highlight the dire need for novel agents in this disease setting. Patients will be randomized to either cystoscopy at 3 months, 12 months and then annually for 5 years versus cystoscopy every 3 months for 2 years, every 6 months for 2 years and annually thereafter. The primary objectives of this study include development of methodology to assess both patient satisfaction and costs associated with cystoscopy for bladder cancer surveillance with secondary objectives of cost, number of overall procedures and proportion of patients with disease recurrence and progression at two years. Agency for Healthcare Research and Quality: Methods guide for effectiveness and comparative effectiveness reviews. Agency for Healthcare Research and Quality: Methods guide for medical test reviews. Faraday M, Hubbard H, Kosiak B et al: Staying at the cutting edge: a review and analysis of evidence reporting and grading; the recommendations of the American Urological Association. Aldousari S and Kassouf W: Update on the management of non-muscle invasive bladder cancer.